Nephrotic Syndrome in Children
On this page:
- What is nephrotic syndrome?
- How common is nephrotic syndrome in children?
- What are the complications of nephrotic syndrome in children?
- What are the signs or symptoms of nephrotic syndrome in children?
- What causes nephrotic syndrome in children?
- How do health care professionals diagnose nephrotic syndrome in children?
- How do health care professionals treat nephrotic syndrome in children?
- How can nephrotic syndrome in children be prevented?
- How do eating, diet, and nutrition affect nephrotic syndrome in children?
- Clinical Trials for Nephrotic Syndrome in Children
What is nephrotic syndrome?
Nephrotic syndrome is a group of symptoms that indicate the kidneys are not working properly. These symptoms include
- too much protein in the urine, called proteinuria
- low levels of a protein called albumin in the blood, called hypoalbuminemia
- swelling in parts of the body, called edema
- high levels of cholesterol and other lipids (fats) in the blood, called hyperlipidemia
The kidneys are made up of about a million filtering units called nephrons. Each nephron includes a filter, called the glomerulus, and a tubule. The glomerulus filters the blood, and the tubule returns needed substances to the blood and removes wastes and extra water, which become urine. Nephrotic syndrome usually happens when the glomeruli are damaged, allowing too much protein to leak from the blood into the urine.
View full-sized image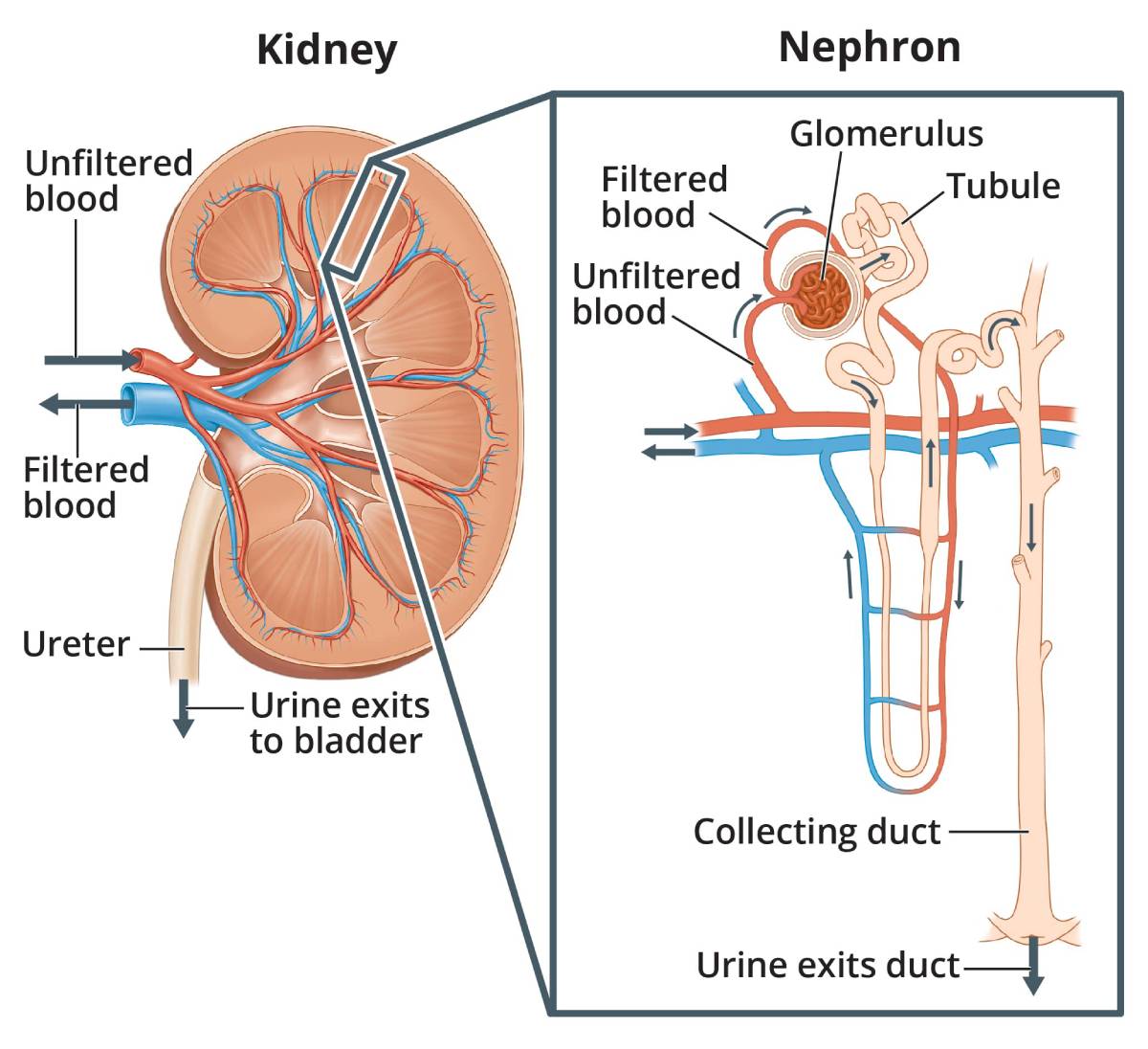 As blood passes through healthy kidneys, the glomeruli filter out waste products and allow the blood to keep the cells and proteins the body needs.
As blood passes through healthy kidneys, the glomeruli filter out waste products and allow the blood to keep the cells and proteins the body needs.
Does nephrotic syndrome in children have another name?
Health care professionals use different terms to refer to nephrotic syndrome in children, depending on
- how old the child is when symptoms begin
- congenital nephrotic syndrome—birth to 3 months
- infantile nephrotic syndrome—3 to 12 months
- childhood nephrotic syndrome—12 months or older
- the cause of nephrotic syndrome
- primary nephrotic syndrome—the syndrome is caused by a kidney disease that affects only the kidneys
- secondary nephrotic syndrome—the syndrome develops because of other causes, such as diseases that affect other parts of the body, infections, and medicines
How common is nephrotic syndrome in children?
Nephrotic syndrome is not very common in children. On average, fewer than 5 in 100,000 children worldwide develop nephrotic syndrome each year.1
 Children of all ages can develop nephrotic syndrome.
Children of all ages can develop nephrotic syndrome.
Which children are more likely to develop nephrotic syndrome?
Children of all ages can develop nephrotic syndrome. But the condition most often affects children who are 2 to 7 years old, particularly boys.2
What are the complications of nephrotic syndrome in children?
Losing too much protein in the urine can lead to many complications, including3
- higher risk of infection
- blood clots
- high blood pressure, also called hypertension
- high cholesterol
- brief or long-lasting kidney problems
What are the signs or symptoms of nephrotic syndrome in children?
Swelling around the eyes is the most common sign of nephrotic syndrome in children.3 The swelling is usually greater in the morning and, when mild, may be confused with seasonal allergies.
Other common symptoms include2,3
- swelling in the lower legs, feet, abdomen, hands, face, or other parts of the body
- foamy urine
- fatigue
Some children with nephrotic syndrome may also have
- blood in their urine
- loss of appetite
- muscle cramps
- diarrhea or nausea
What causes nephrotic syndrome in children?
Kidney disease that affects a kidney’s filtering system is the most common cause of nephrotic syndrome in children. Other causes can include diseases that affect other parts of the body, infections, some medicines, and genetics.
Primary nephrotic syndrome
Four types of kidney disease can cause primary nephrotic syndrome in children and adolescents.2
- Minimal change disease (MCD). MCD is the most common cause of nephrotic syndrome in young children. The disease causes very little change to the glomeruli or nearby kidney tissue. The changes in the kidney can only be seen using an electron microscope, which shows tiny details. Although the cause of MCD is unknown, some health care professionals think the immune system may be involved.
- Focal segmental glomerulosclerosis (FSGS). This disease can cause some of the kidney’s glomeruli to become scarred. FSGS may be caused by genetic variants, or changes in genes present at birth.
- Membranous nephropathy (MN). MN is an autoimmune disease that causes immune proteins to build up in the kidney’s glomerular basement membrane. As a result, the membrane becomes thick and does not work properly, allowing too much protein to pass into the urine.
Other causes of primary nephrotic syndrome are uncommon.
Secondary nephrotic syndrome
Causes of secondary nephrotic syndrome in children include3
- diseases that involve many organs or the whole body, called systemic diseases. Examples include IgA vasculitis (also known as Henoch-Schönlein purpura) and lupus.
- infections, including hepatitis B and C, HIV, and malaria.
- diseases of the blood, such as leukemia, lymphoma, and sickle cell disease.
- some medicines and drugs, such as nonsteroidal anti-inflammatory drugs, and some medicines used to treat mood disorders, bone loss, or cancer.
Congenital nephrotic syndrome
Among newborns and infants younger than 12 months old, the two most common causes of nephrotic syndrome are4
- genetic variants, which account for most cases of congenital nephrotic syndrome
- infections present at or before birth, such as syphilis and toxoplasmosis
How do health care professionals diagnose nephrotic syndrome in children?
Nephrotic syndrome in children is diagnosed with
- a medical and family history
- a physical exam
- urine tests, to look for excess urine proteins
- blood tests, to test kidney function and to look for underlying diseases
Additional tests to identify the cause of nephrotic syndrome may include3
- ultrasound of the kidney
- kidney biopsy
- genetic testing
Many children with nephrotic syndrome will not need a kidney biopsy. The test is usually reserved for children who have complex disease, who have low kidney function, or who are 12 years old or older.3
How do health care professionals treat nephrotic syndrome in children?
Nephrotic syndrome in children is most often treated with medicines.
Primary nephrotic syndrome
Corticosteroids. Corticosteroids, or steroids, are the medicines most often used to treat children with primary nephrotic syndrome. These medicines suppress the immune system, reduce the amount of protein passed into the urine, and decrease swelling.
In most children, treatment with corticosteroids will make nephrotic syndrome improve—also called “remission.” If symptoms return, called a “relapse,” the health care professional may prescribe a shorter course of corticosteroids until the disease goes into remission again. Although children may have multiple relapses, they often recover without long-term kidney damage. In most cases, relapses happen less often as children get older.3
Although corticosteroids effectively treat nephrotic syndrome in many children, using these medicines for long periods of time can cause side effects, such as impaired growth, obesity, high blood pressure, eye problems, and bone loss.3 Other common side effects include anxiety, depression, and aggressive behavior. These problems are more likely to develop with larger doses and longer use.
In some cases, nephrotic syndrome may not improve with corticosteroids. Cases of nephrotic syndrome that don’t respond to corticosteroids are more difficult to treat than those that do. They are also more likely to progress to end-stage kidney disease.3
Other medicines that suppress the immune system. If corticosteroids are not working or are causing harmful side effects, your child’s health care professional may prescribe other medicines that reduce the activity of the immune system. In some cases, your child may take these medicines together with low-dose corticosteroids.
Medicines for managing symptoms and complications. Health care professionals may also prescribe other medicines to help your child manage the symptoms and complications of nephrotic syndrome. Examples include
- angiotensin-converting enzyme (ACEs) inhibitors or angiotensin receptor blockers (ARBs) to lower blood pressure and help reduce protein loss
- diuretics, or water pills, to reduce swelling by helping the kidneys remove extra fluid from the blood
- statins to lower cholesterol
- blood thinners to treat blood clots
Children with nephrotic syndrome should get the pneumococcal vaccine and yearly flu shots to prevent viral and bacterial infections. They should also get age-appropriate vaccinations. But the health care professional may delay certain “live” vaccines—vaccines that use weakened forms of a virus—while your child is taking certain medicines.
Secondary nephrotic syndrome
Treatment focuses on the cause of nephrotic syndrome. For example, the health care professional may
- prescribe antibiotics to treat an infection that may be causing nephrotic syndrome
- change or stop any medicines your child takes that can cause nephrotic syndrome or make it worse, such as some medicines used to treat lupus, HIV, or diabetes
Your child’s health care professional may also prescribe the same medicines used to manage the symptoms and complications of primary nephrotic syndrome.
Congenital nephrotic syndrome
Treatment varies depending on whether the cause is genetic or an infection.
Genetic. Your child’s treatment will depend on the type of genetic mutation that is causing nephrotic syndrome and how bad the symptoms and complications are. Many children will lose kidney function over time and ultimately need a kidney transplant. To keep your child healthy until the transplant, the health care professional may recommend4,5
- albumin injections to make up for the albumin passed in urine
- medicines to reduce swelling, lower blood pressure, and reduce protein loss
- removal of one or both kidneys to decrease the loss of albumin in the urine
- dialysis to filter wastes from the blood if the kidneys fail or if both kidneys are removed
Infection. When nephrotic syndrome is caused by a congenital infection, such as syphilis or toxoplasmosis, it will usually go away when the infection is treated.4
How can nephrotic syndrome in children be prevented?
Researchers have not found a way to prevent nephrotic syndrome in children. Knowing the symptoms can help you get your child treated early and reduce the risk of complications.
How do eating, diet, and nutrition affect nephrotic syndrome in children?
Children who have nephrotic syndrome may need to change what they eat and drink, such as
- limiting the amount of sodium they get, often from salt
- reducing the amount of liquid they drink
- eating foods low in saturated fat and cholesterol
In some cases, the child’s health care professional may recommend other dietary changes. Parents or other caregivers should talk with their child’s health care professional before making any changes to the child’s diet.
Clinical Trials for Nephrotic Syndrome in Children
The NIDDK conducts and supports clinical trials in many diseases and conditions, including kidney diseases. The trials look to find new ways to prevent, detect, or treat disease and improve quality of life.
Why are clinical trials with children important?
Children respond to medicines and treatments differently than adults. The way to get the best treatments for children is through research designed specifically for them.
We have already made great strides in improving children's health outcomes through clinical trials—and other types of clinical studies. Vaccines, treatments for children with cancer, and interventions for premature babies are just a few examples of how this targeted research can help. However, we still have many questions to answer and more children waiting to benefit.
The data gathered from trials and studies involving children help doctors and researchers
- find the best dose of medicines for children
- find treatments for conditions that only affect children
- treat conditions that behave differently in children than in adults
- understand the differences in children as they grow
How do I decide if a clinical trial is right for my child?
We understand you have many questions, want to weigh the pros and cons, and need to learn as much as possible. Deciding to enroll in a study can be life changing for you and for your child. Depending on the outcome of the study, your child may find relief from their condition, see no benefit, or help to improve the health of future generations.
Talk with your child and consider what would be expected. What could be the potential benefit or harm? Would you need to travel? Is my child well enough to participate? While parents or guardians must give their permission, or consent, for their children to join a study, the children must also agree to participate, if they are capable (verbal). In the end, no choice is right or wrong. Your decision is about what is best for your child.
The National Institutes of Health (NIH) is committed to ensuring you get all the information you need to feel comfortable and make informed decisions. The safety of children remains the utmost priority for all NIH research studies. For more resources to help decide if clinical trials are right for your child, visit Clinical Trials and You: For Parents and Children.
What aspects of nephrotic syndrome are being studied in children?
Researchers study many aspects of nephrotic syndrome in children, such as the kidney diseases that can cause nephrotic syndrome in children and the genetic factors that can cause congenital nephrotic syndrome.
Watch a video of NIDDK Director Dr. Griffin P. Rodgers explaining the importance of participating in clinical trials.
What clinical studies for nephrotic syndrome are available for child participants?
You can view a filtered list of clinical studies on nephrotic syndrome in children that are federally funded, open, and recruiting at ClinicalTrials.gov. You can expand or narrow the list to include clinical studies from industry, universities, and individuals; however, the NIH does not review these studies and cannot ensure they are safe. If you find a trial you think may be right for your child, talk with your child’s doctor about how to enroll.
References
This content is provided as a service of the National Institute of Diabetes and Digestive and Kidney Diseases
(NIDDK), part of the National Institutes of Health. NIDDK translates and disseminates research findings to increase knowledge and understanding about health and disease among patients, health professionals, and the public. Content produced by NIDDK is carefully reviewed by NIDDK scientists and other experts.
The NIDDK would like to thank:
Debbie Gipson, M.D., University of Michigan Medical School
