Medullary Sponge Kidney
On this page:
- What is Medullary Sponge Kidney?
- What are the complications of Medullary Sponge Kidney?
- What causes Medullary Sponge Kidney?
- How common is Medullary Sponge Kidney?
- Who is more likely to develop Medullary Sponge Kidney?
- What are the signs and symptoms of Medullary Sponge Kidney?
- How is Medullary Sponge Kidney diagnosed?
- How is Medullary Sponge Kidney treated?
- Can Medullary Sponge Kidney be prevented?
- Medications to Prevent Future Urinary Tract Infections and Kidney Stones
- Eating, Diet, and Nutrition
- Clinical Trials
What is Medullary Sponge Kidney?
Medullary sponge kidney, also known as Cacchi-Ricci disease, is a birth defect where changes occur in the tubules, or tiny tubes, inside a fetus’ kidneys. Advisory Council Minutes (PDF, 385.25 KB)
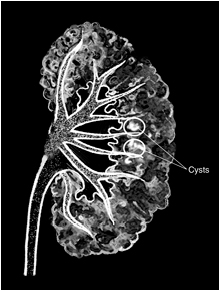
In a normal kidney, urine flows through these tubules as the kidney is being formed during a fetus’ growth. In medullary sponge kidney, tiny, fluid-filled sacs called cysts form in the tubules within the medulla—the inner part of the kidney—creating a spongelike appearance. The cysts keep urine from flowing freely through the tubules.
Symptoms of medullary sponge kidney do not usually appear until the teenage years or the 20s. Medullary sponge kidney can affect one or both kidneys.
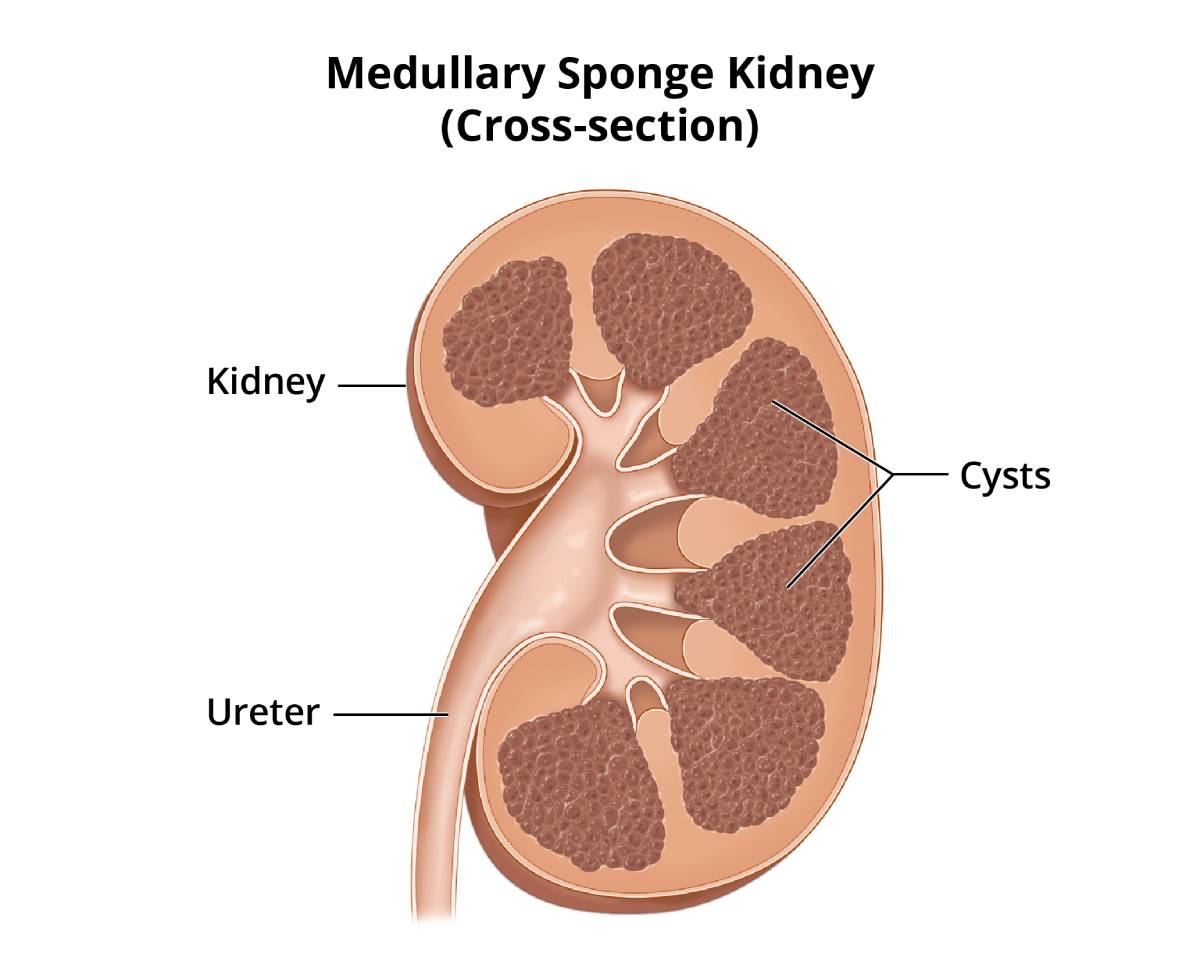 View full-sized image
View full-sized image What are the complications of Medullary Sponge Kidney?
Complications of medullary sponge kidney include
Medullary sponge kidney rarely leads to more serious problems, such as chronic kidney disease or kidney failure.
What causes Medullary Sponge Kidney?
Scientists do not fully understand the cause of medullary sponge kidney or why cysts form in the tubules during fetal development. Even though medullary sponge kidney is present at birth, most cases do not appear to be inherited.
How common is Medullary Sponge Kidney?
Medullary sponge kidney affects about one person per 5,000 people in the United States. Researchers have reported that 12 to 20 percent of people who develop calcium-based kidney stones have medullary sponge kidney.1
Who is more likely to develop Medullary Sponge Kidney?
Medullary sponge kidney affects all races and geographic regions. Among people who are more likely to develop calcium-based kidney stones, women are more likely than men to have medullary sponge kidney.2
What are the signs and symptoms of Medullary Sponge Kidney?
Many people with medullary sponge kidney have no symptoms. The first sign that a person has medullary sponge kidney is usually a UTI or a kidney stone. UTIs and kidney stones share many of the same signs and symptoms:
- burning or painful urination
- pain in the back, lower abdomen, or groin
- cloudy, dark, or bloody urine
- foul-smelling urine
- fever and chills
- vomiting
People who experience these symptoms should see or call a health care provider as soon as possible.
How is Medullary Sponge Kidney diagnosed?
A health care provider diagnoses medullary sponge kidney based on
- a medical and family history
- a physical exam
- imaging studies
Medical and Family History
Taking a medical and family history can help diagnose medullary sponge kidney. A health care provider will suspect medullary sponge kidney when a person has repeated UTIs or kidney stones.
Physical Exam
No physical signs are usually present in a patient with medullary sponge kidney, except for blood in the urine. Health care providers usually confirm a diagnosis of medullary sponge kidney with imaging studies.
Imaging Studies
Imaging is the medical term for tests that use different methods to see bones, tissues, and organs inside the body. Health care providers commonly choose one or more of three imaging techniques to diagnose medullary sponge kidney:
- intravenous pyelogram
- computerized tomography (CT) scan
- ultrasound
A radiologist—a doctor who specializes in medical imaging—interprets the images from these studies, and patients do not need anesthesia.
Intravenous Pyelogram
In an intravenous pyelogram, a health care provider injects a special dye, called contrast medium, into a vein in the patient’s arm. The contrast medium travels through the body to the kidneys. The kidneys excrete the contrast medium into urine, which makes the urine visible on an x-ray. An x-ray technician performs this procedure at a health care provider’s office, an outpatient center, or a hospital. An intravenous pyelogram can show any blockage in the urinary tract, and the cysts show up as clusters of light.
Computerized Tomography Scans
Computerized tomography scans use a combination of x-rays and computer technology to create images. For a CT scan, a health care provider may give the patient a solution to drink and an injection of contrast medium. CT scans require the patient to lie on a table that slides into a tunnel-shaped device where the x-rays are taken. An x-ray technician performs the procedure in an outpatient center or a hospital. CT scans can show expanded or stretched tubules.
Ultrasound
Ultrasound uses a device, called a transducer, that bounces safe, painless sound waves off organs to create an image of their structure. A specially trained technician performs the procedure in a health care provider’s office, an outpatient center, or a hospital. Ultrasound can show kidney stones and calcium deposits within the kidney.
How is Medullary Sponge Kidney treated?
Scientists have not discovered a way to reverse medullary sponge kidney. Once a health care provider is sure a person has medullary sponge kidney, treatment focuses on
- curing an existing UTI
- removing any kidney stones
Curing an Existing Urinary Tract Infection
To treat a UTI, the health care provider may prescribe a medication called an antibiotic that kills bacteria. The choice of medication and length of treatment depend on the person’s medical history and the type of bacteria causing the infection.
Removing Kidney Stones
Treatment for kidney stones usually depends on their size and what they are made of, as well as whether they are causing pain or obstructing the urinary tract. Kidney stones may be treated by a general practitioner or by a urologist—a doctor who specializes in the urinary tract.
Small stones usually pass through the urinary tract without treatment. Still, the person may need pain medication and should drink lots of liquids to help move the stone along. Pain control may consist of oral or intravenous (IV) medication, depending on the duration and severity of the pain. People may need IV fluids if they become dehydrated from vomiting or an inability to drink.
A person with a larger stone, or one that blocks urine flow and causes great pain, may need more urgent treatment, such as
- shock wave lithotripsy. A machine called a lithotripter is used to break up the kidney stone into smaller pieces to pass more easily through the urinary tract. The patient may need local or general anesthesia.
- ureteroscopy. A ureteroscope—a long, tubelike instrument with an eyepiece—is used to find and retrieve the stone with a small basket or to break the stone up with laser energy. Local or general anesthesia may be required.
- percutaneous nephrolithotomy. In this procedure, a wire-thin viewing instrument, called a nephroscope, is used to locate and remove the stones. During the procedure, which requires general anesthesia, a tube is inserted directly into the kidney through a small incision in the patient’s back.
Can Medullary Sponge Kidney be prevented?
Scientists have not yet found a way to prevent medullary sponge kidney. However, health care providers can recommend medications and dietary changes to prevent future UTIs and kidney stones.
Medications to Prevent Future Urinary Tract Infections and Kidney Stones
Health care providers may prescribe certain medications to prevent UTIs and kidney stones:
- A person with medullary sponge kidney may need to continue taking a low-dose antibiotic to prevent recurrent infections.
- Medications that reduce calcium in the urine may help prevent calcium kidney stones. These medications may include
- potassium citrate
- thiazide
Eating, Diet, and Nutrition
The following changes in diet may help prevent UTIs and kidney stone formation:
- Drinking plenty of water and other liquids can help flush bacteria from the urinary tract and dilute urine so kidney stones cannot form. A person should drink enough liquid to produce about 2 to 2.5 quarts of urine every day.3
- Reducing sodium intake, mostly from salt, may help prevent kidney stones. Diets high in sodium can increase the excretion of calcium into the urine and thus increase the chance of calcium-containing kidney stones forming.
- Foods rich in animal proteins such as meat, eggs, and fish can increase the chance of uric acid stones and calcium stones forming. People who form stones should limit their meat consumption to 6 to 8 ounces a day.4
- People who are more likely to develop calcium oxalate stones should include 1,000 milligrams of calcium in their diet every day. Adults older than 50 years should consume 1,200 milligrams of calcium daily.3 Calcium in the digestive tract binds to oxalate from food and keeps it from entering the blood and the urinary tract, where it can form stones.
People with medullary sponge kidney should talk with their health care provider or a dietitian before making any dietary changes. A dietitian can help a person plan healthy meals.
Clinical Trials
The National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) and other components of the National Institutes of Health (NIH) conduct and support research into many diseases and conditions.
What are clinical trials, and are they right for you?
Clinical trials are part of clinical research and at the heart of all medical advances. Clinical trials look at new ways to prevent, detect, or treat disease. Researchers also use clinical trials to look at other aspects of care, such as improving the quality of life for people with chronic illnesses. Find out if clinical trials are right for you.
What clinical trials are open?
Clinical trials that are currently open and are recruiting can be viewed at ClinicalTrials.gov.
References
This content is provided as a service of the National Institute of Diabetes and Digestive and Kidney Diseases
(NIDDK), part of the National Institutes of Health. NIDDK translates and disseminates research findings to increase knowledge and understanding about health and disease among patients, health professionals, and the public. Content produced by NIDDK is carefully reviewed by NIDDK scientists and other experts.
The NIDDK would like to thank:
Deepa Chand, M.D., Akron Children’s Hospital; Maria Ferris, M.D., University of North Carolina; Joseph Flynn, M.D., M.S., Seattle Children’s Hospital; Keith Lau, M.D., McMaster University, Hamilton, Ontario; Tej Mattoo, M.D., Children’s Hospital of Michigan, Detroit; Asha Mougdil, M.D., Children’s National Medical Center, Washington, D.C.; and Robert Weiss, M.D., Maria Fareri Children’s Hospital, all members of the American Society of Pediatric Nephrology Clinical Affairs Committee
