Research Updates

NIH study finds heavily processed foods cause overeating and weight gain: People eating ultra-processed foods ate more calories and gained more weight than when they ate a minimally processed diet, an NIH study found. The small-scale trial was the first randomized, controlled research to compare the health effects of ultra-processed and unprocessed diets. The diets were defined by the NOVA classification system, which considers foods “ultra-processed” if they have ingredients predominantly found in industrial food manufacturing, such as hydrogenated oils, high-fructose corn syrup, flavoring agents, and emulsifiers. The study was published in May in Cell Metabolism.
Early weight-loss surgery may improve type 2 diabetes, blood pressure outcomes: Despite similar weight loss, teens who had weight-loss surgery were significantly more likely to have reversed both type 2 diabetes and high blood pressure, compared to adults who had the same procedure. Previously, no treatment has shown longer-term effectiveness at reversing type 2 diabetes in youth, which tends to advance more quickly than in adults. Researchers evaluated 161 teens and 396 adults who underwent gastric bypass surgery at clinical centers participating in the NIDDK-funded Teen-LABS (Teen-Longitudinal Assessment of Bariatric Surgery) and compared results with its adult counterpart, LABS, five years after surgery. Teens in the study were under 19 years old at the time of surgery, and adults in the study reported having obesity by age 18. The results were published in The New England Journal of Medicine in May.
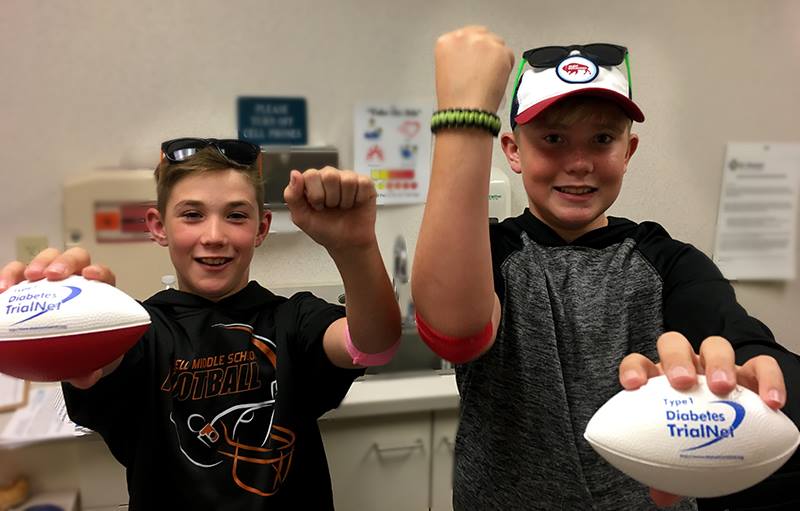
Drug delays type 1 diabetes in people at high risk: A treatment affecting the immune system effectively slowed the progression to type 1 diabetes in high-risk people, according to findings from the NIH-supported Type 1 Diabetes TrialNet. The study is the first to show that clinical type 1 diabetes can be delayed by two or more years among people who are at high risk. The study involved treatment with an anti-CD3 monoclonal antibody (teplizumab). It enrolled 76 participants ages 8-49 who were relatives of people with clinical type 1 diabetes, had at least two types of diabetes-related autoantibodies, and abnormal glucose tolerance. Participants were randomly assigned to either the treatment group, which received a 14-day course of teplizumab, or the control group, which received a placebo. During the trial, 72% of people in the control group developed diabetes, compared to only 43% of the teplizumab group. The median time for people in the control group to develop diabetes was just over 24 months, while those who developed diabetes in the treatment group had a median time of 48 months before progressing to diagnosis. These results were published in June in The New England Journal of Medicine and presented at the 2019 American Diabetes Association Scientific Sessions in San Francisco.
"Wildling" mice could help translate results in animal models to results in humans: NIH researchers created a new mouse model by transplanting embryos of laboratory mice into female wild mice, who gave birth to a colony of mice the researchers called wildlings. The wildlings acquired the microbes and pathogens of wild mice, while maintaining the laboratory mice’s genetics that make them more useful for research. In two preclinical studies, wildlings mirrored human immune responses, where lab mice failed to do so. Led by scientists in NIDDK’s Liver Diseases Branch, the study published online in Science in August.
Daily folic acid supplement may reduce risk of gestational diabetes: Taking a daily folic acid supplement before pregnancy may not only reduce the risk of birth defects, but also reduce the risk of gestational (pregnancy-related) diabetes, according to a study by researchers at the National Institutes of Health and other institutions.
In the current study, researchers analyzed data from nearly 15,000 women enrolled in the Nurses’ Health Study II, a long-term study of diet, lifestyle factors and disease outcomes among female nurses. Among more than 20,000 pregnancies, there were 824 cases of gestational diabetes. Compared to women who did not take a folic acid supplement, those who took less than 400 micrograms were 22% less likely to develop gestational diabetes. Those who took 600 micrograms were 30% less likely to develop the condition. The researchers did not find a lower risk of gestational diabetes associated with consumption of foods that contain high amounts of folate. The findings appeared in Diabetes Care in June.
Early life gluten consumption a risk factor for celiac disease in children at high genetic risk: An international team of researchers from The Environmental Determinants of Diabetes in the Young (TEDDY) study have found that consuming higher levels of gluten daily during the first 5 years of life was associated with an increased risk of developing celiac disease autoimmunity or celiac disease. The study included 6,605 children who were screened as infants and found to be at high genetic risk for celiac disease. After a median of 9 years of follow up, 18% developed celiac disease autoimmunity and 7% developed celiac disease. Daily gluten intake was associated with higher risk of celiac disease autoimmunity and celiac disease with as little as a 1-gram per day increase of gluten consumption. Among the cohort, incidence of both conditions peaked when participants reached 2 to 3 years of age. These results were published in the Journal of the American Medical Association in August.
The Human Microbiome Project expands the toolbox for studying host and microbiome interactions: A recent project led by researchers at Stanford University and the Jackson Laboratory for Genomic Medicine followed the dynamic interplay of the host with gut and nasal microbiomes in the development of type 2 diabetes. The study team followed 106 participants for nearly four years. When the study began, 51 participants had prediabetes and a portion of the participants had insulin resistance.
Many specimens were collected from the participants over time and analyzed for changes in the microbiome, as well as several other molecular processes in the body. Particular attention was dedicated to changes that could have been caused by challenges to the immune system like viral respiratory infections. Extensive differences were identified in molecular pathway changes in participants with respiratory infections. Some pathways involved in the immune response seemed abnormal during respiratory infections in insulin resistant participants versus insulin sensitive. While the study is small, it highlights the complex and dynamic interaction between host and microbes during health and immune disruptions. This work, published in Nature in May, is part of the NIH Human Microbiome Project, funded by the NIH Common Fund.

NIH-funded trial finds vitamin D does not prevent type 2 diabetes in people at high risk: Taking a daily vitamin D supplement does not prevent type 2 diabetes in adults at high risk, according to results from the Vitamin D and Type 2 Diabetes (D2d) study, funded by NIDDK. D2d is the largest study to directly examine if daily vitamin D supplementation helps keep people at high risk for type 2 diabetes from developing the disease. The study enrolled 2,423 adults aged 30 or older at 22 sites across the United States and assigned them randomly to either take 4,000 International Units (IU) of the D3 (cholecalciferol) form of vitamin D or a placebo pill daily. At the end of the study, 293 out of 1211 participants (24.2%) in the vitamin D group developed diabetes compared to 323 out of 1212 (26.7%) in the placebo group – a difference that did not reach statistical significance. Because of the popularity of vitamin D supplements in the U.S., the study also evaluated the safety of taking 4,000 units of vitamin D daily. The researchers saw no difference in the number and frequency of side effects, such as high blood calcium levels and kidney stones when compared to the vitamin D and placebo groups. These findings were published in the New England Journal of Medicine and presented at the 79th Scientific Sessions of the American Diabetes Association in San Francisco.
Lack of protein β-arrestin-2 in adipocytes associated with pronounced metabolic improvements in mice. Research led by scientists at NIDDK found that mice lacking the β-arrestin-2 protein in adipocytes, cells specialized in the storage of fat, showed decreased body weight, fat mass, and blood glucose levels, and increased glucose and insulin tolerance when maintained on a high fat diet. The researchers also found that these metabolic improvements were associated with the browning of white fat and increased energy expenditure.
This research was the first to show the β-arrestin-2 protein as a critical regulator of whole-body glucose and energy homeostasis in adipocytes. G proteins, a family of proteins that transmit signals to a cell’s interior, also played a role in this research. Data from this study support the novel concept that G protein-biased agonists of β3-adrenergic receptors, located mainly in adipose tissue and involved in promoting lipolysis, that do not promote interactions with β-arrestin-2 may prove clinically useful for the treatment of obesity and related metabolic disorders. This research was published in Nature Communications in July.
Exome sequencing of 20,791 cases of type 2 diabetes and 24,440 controls: An international consortium of scientists has analyzed the exomes of early 46,000 people, linking rare DNA alterations to type 2 diabetes. The study, one of the largest of its type, includes data from people of European, African American, Hispanic/Latino, East Asian, and South Asian ancestries. From this large cohort—roughly 21,000 individuals with type 2 diabetes and 25,000 healthy controls—the researchers identified four genes with rare variants that affect diabetes risk. The data suggests that hundreds more genes will likely be identified in the future. This study illustrates the importance of utilizing exome sequencing in addition to genome-wide association studies to comprehensively study the underlying biology of complex disease traits. While rare exome variants are difficult to detect, they can provide invaluable insight into disease-related genes, which in turn can suggest new drug targets. This work, part of the Accelerating Medicines Partnership® in Type 2 Diabetes (AMP® T2D) program, was published in Nature in April.

Improvements in insulin release wane after treatment stops in adults with early type 2 diabetes: A set of clinical trials examining youth and adults with type 2 diabetes or impaired glucose tolerance has found that disease progression in adults slowed during medical treatment but resumed after treatment stopped. Youth on the same treatment had markedly poorer outcomes with continued disease progression both during and after the treatment.
The Restoring Insulin Secretion (RISE) Adult and Pediatric Medication Studies compared the use of different treatments among adults ages 20-65 and youth ages 10-19 with impaired glucose tolerance or early onset type 2 diabetes with the aim of preserving beta cell function – key to the body’s ability to make and release insulin. Results, published in Diabetes Care, showed that adult participants had improvements in beta cell function and blood glucose control while on the treatments, with those in the liraglutide plus metformin group showing the most improvement after 12 months. However, these improvements did not persist among any of the groups after treatment ended.
In a companion paper, published in Diabetes, findings from the adult study were compared to those from the RISE Pediatric Medication Study published in 2018, which showed that beta cell function declined in the two youth treatment groups during active treatment, and worsened after treatment ended. Both papers were published in June and findings presented at the American Diabetes Association Scientific Sessions in San Francisco.
Artificial sweetener exposure caused metabolic changes in baby mice. NIDDK researchers found that exposure to non-nutritive sweeteners via the placenta and breast milk led to metabolic and microbiome abnormalities in baby mice. The researchers fed pregnant and lactating mice one of two sweetener solutions and analyzed the effects on their pre-weaned pups. The solutions were a mixture of sucralose and acesulfame-K at the 'acceptable daily intake' (ADI), double the ADI, or a control (water). The ADI is the maximum consumption deemed safe for human consumption by the Food and Drug Administration based on toxicology studies. The mouse pups in both ADI groups showed significant metabolic changes compared to the control group. These changes indicated impaired liver functioning in clearing toxins from the blood and a dramatic shift in bacterial metabolites in the gut. For example, the researchers observed the loss of a major beneficial species of gut bacteria, Akkermansia muciniphila. Similar microbiome alterations in humans have been linked to type 2 diabetes and obesity. The results suggest that pre- and post-natal exposure to artificial sweeteners could adversely affect detoxification systems and the microbiome, as well as increase susceptibility to metabolic disease. The study was published in Frontiers in Microbiology on June 20.

Watchful waiting reasonable for patients with diabetic macular edema and good vision: People with good vision despite having center-involved diabetic macular edema can safely forego immediate treatment of their eye condition as long as they are closely monitored, and treatment begins promptly if vision worsens, according to recent clinical trial results. The study was conducted by the DRCR Retina Network, a multicenter clinical research network funded by NIH.
Diabetic macular edema is the most common cause of vision loss among people with diabetic eye disease in the United States and is the result of fluid build-up in the central area of the retina, called the macula, which is important for sharp vision. The evidence from this study should help physicians and patients navigate a common conundrum in ophthalmology: Treating diabetic macular edema in people who still have good vision too soon may subject them to unnecessary costs and risks associated with treatment. Other patients who get treatment too late might risk losing vision permanently. The findings are published online in the Journal of the American Medical Association.
Gout treatment may help prevent obesity-related type 2 diabetes: The drug colchicine, used to treat the arthritic condition gout, could potentially reduce complications accompanying metabolic syndrome, a combination of high blood pressure, high blood sugar and other conditions that increase the risk of heart disease and type 2 diabetes, according to NIH researchers.
Previous studies have indicated that the system-wide inflammation that occurs in obesity plays a role in the development of type 2 diabetes. In the current study, researchers randomly assigned 21 study participants to receive colchicine twice a day for 3 months, while 19 participants received a placebo. Colchicine suppresses a multi-protein complex called NLRP3, which triggers the inflammation seen in obesity. There was no difference between the two groups in insulin resistance determined by one measure of assessment (the frequently sampled, insulin-modified intravenous glucose tolerance test). However, the colchicine group showed improvement on the Homeostatic Model Assessment of Insulin Resistance test, another assessment of how much insulin is needed to keep blood sugar at a normal level while fasting. Those in the colchicine group also scored lower on a blood test of C-reactive protein and other tests that indicate inflammation. Their study appeared in Diabetes, Endocrinology, and Metabolism in July.
Gene variants associated with BMI and diabetes in Pacific Islanders. Research led by scientists at NIDDK’s Phoenix Epidemiology and Clinical Research Branch found that variants in the CREBRF gene were linked to higher BMI and lower risk of type 2 diabetes in populations from Guam and Saipan. The researchers also observed that the gene variants were moderately associated with taller height. These findings reflect results from earlier studies, which showed that the same CREBRF variants were associated with higher BMI and lower type 2 diabetes risk in Polynesian populations. This gene variant is common in Polynesians and appears in low frequencies among the Mariana and Micronesian populations included in the current study. However, in most other global populations, the variant is nearly non-existent.
Further investigation is needed into the mechanism behind the seemingly conflicting association of higher obesity but lower diabetes risk. The present study suggests that the gene variant does not modify the effect of BMI on diabetes risk, but that it separately lower diabetes risk while increasing BMI. Expanding on this research to better understand how the CREBRF gene works could inform new avenues of treatment of obesity and diabetes. The study was published online in Diabetologia on July 6.
Being teased about weight may lead to more weight gain among children: In a recent study, youth who said they were teased or ridiculed about their weight increased their body mass by 33% more each year, compared to youth who were not teased. NIH researchers surveyed 110 youth with an average age of about 12 years old who were either overweight or had two parents who were overweight or obese. The youth completed a six-item questionnaire on whether they had been teased about their weight, and researchers followed up with them for the next 15 years. The youth who experienced high levels of teasing gained an average of about 0.44 pounds more per year than those who were not teased as much. The study’s authors suggested that weight-associated stigma may have made youth more likely to binge eat and avoid exercise, or that the stress of being teased could have stimulated the release of the hormone cortisol, which can lead to weight gain. The study was published in May in Pediatric Obesity.
NIH publishes the largest genomic study on type 2 diabetes in sub-Saharan African populations: NIH researchers and colleagues have reported the largest genomic study of type 2 diabetes (T2D) in sub-Saharan Africans, with data from more than 5,000 individuals from Nigeria, Ghana and Kenya. Researchers confirmed known genomic variants and identified a novel gene, known as ZRANB3, which may influence susceptibility to the disease in sub-Saharan African populations.
In the study, published in the journal Nature Communications in July, researchers analyzed genomic data available on participants through the African America Diabetes Mellitus study, the single largest diabetes genomic association study conducted on the continent. Using the information available from 5,231 people, they found many genomic variants to be significantly associated with T2D, replicating results from mostly European ancestry populations. To better understand the role of ZRANB3 in the development of type 2 diabetes, the researchers studied the effects of the gene in the zebrafish pancreas and in mouse beta cells. They found that inactivation of the gene caused beta cell death and reduced beta cell function in the zebrafish and mouse model, respectively. While the role of ZRANB3 in T2D was discovered in African populations, more research is needed to determine whether the same gene may influence the development of T2D in other populations.

Long-term weight loss with metformin or lifestyle intervention in the Diabetes Prevention Program Outcomes Study: Researchers from the Diabetes Prevention Program Outcome Study (DPPOS) evaluated predictors of longer term weight loss (LTWL) over 15 years among 1,066 of the original 3,234 participants enrolled in the original Diabetes Prevention Program (DPP) who had achieved 5% or greater weight loss over the first year of the study. DPP was a multicenter trial examining the ability of intensive lifestyle modification (ILS) or treatment with metformin to prevent or delay the development of type 2 diabetes in individuals at high risk for the disease. Participants assigned to metformin treatment continued to have this drug offered to them in DPPOS. This manuscript found that losing a greater amount of weight over the first year of DPP was a consistent predictor of LWTL regardless of which intervention the person received. However, the group randomized to metformin maintained a greater average percent weight loss over the long-term than the groups who received ILS or placebo. In the group receiving metformin, being of older age and having current use of metformin were found to be important factors in achieving LTWL. Findings from this study were published in April in Annals of Internal Medicine.

