Flexible Sigmoidoscopy
On this page:
- What is flexible sigmoidoscopy?
- How do doctors use flexible sigmoidoscopy?
- How do I prepare for a flexible sigmoidoscopy?
- How do doctors perform a flexible sigmoidoscopy?
- What should I expect after a flexible sigmoidoscopy?
- What are the risks of a flexible sigmoidoscopy?
What is flexible sigmoidoscopy?
Flexible sigmoidoscopy is a procedure in which a doctor uses a flexible tube with a camera on one end, called a sigmoidoscope or scope, to look inside your rectum and lower colon. The lower colon includes the sigmoid colon and descending colon.
Flexible sigmoidoscopy can show irritated or swollen tissue, ulcers, polyps, and cancer.
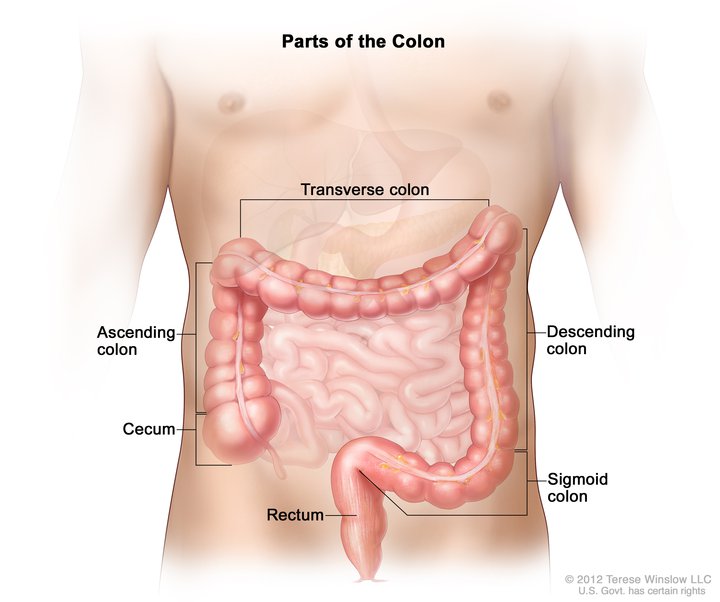 Doctors use flexible sigmoidoscopy to look inside your rectum and the lower part of your colon, including the sigmoid colon and descending colon.
Doctors use flexible sigmoidoscopy to look inside your rectum and the lower part of your colon, including the sigmoid colon and descending colon.
How do doctors use flexible sigmoidoscopy?
A flexible sigmoidoscopy can help a doctor find the cause of symptoms, such as
- bleeding from your anus
- changes in your bowel movements, such as diarrhea
- pain in your abdomen, or belly
- unexplained weight loss
Rarely, doctors also use flexible sigmoidoscopy as a screening tool for colon polyps and colon and rectal cancer—also called colorectal cancer. Screening is testing for diseases when you have no symptoms. Screening may find diseases at an early stage, when a doctor has a better chance of curing the disease.
Screening for colorectal cancer
Your doctor will recommend screening for colorectal cancer at age 45 if you don’t have health problems or risk factors that make you more likely to develop colon cancer.1
You may be more likely to develop colorectal cancer if you1,2
- are age 45 or older
- are Black
- have a personal or family history of colorectal cancer
- have a personal history of ovarian cancer, polyps, or inflammatory bowel disease, such as ulcerative colitis or Crohn’s disease
- have Lynch syndrome or another genetic disorder that increases the risk of colorectal cancer
- have obesity, smoke cigarettes, or drink alcohol
If you are more likely to develop colorectal cancer, your doctor may recommend you get screenings at a younger age and more often.
Flexible sigmoidoscopy is one test used to screen for colorectal cancer. Other screening tests may include
- colonoscopy, a procedure in which a doctor uses a flexible tube with a camera on one end to look inside your rectum and colon
- virtual colonoscopy, a procedure in which a radiologist uses images created by x-rays and a computer to examine your rectum and colon from outside the body
- stool tests that check your stool for blood or changes in your DNA that may be related to colorectal cancer
Doctors may recommend colonoscopy to screen for colorectal cancer because colonoscopy shows the entire colon. However, a flexible sigmoidoscopy may take less time than a colonoscopy. You also may not need sedatives or anesthesia. Your doctor may combine flexible sigmoidoscopy with other tests.
If your doctor finds abnormal tissue or polyps during a flexible sigmoidoscopy, the doctor may recommend a colonoscopy to examine the rest of your colon.
If you are older than age 75, talk with your doctor about whether you should be screened for colorectal cancer. For more information, read the current colorectal cancer screening guidelines from the U.S. Preventive Services Task Force (USPSTF).
Government health insurance plans, such as Medicare, and private health insurance plans sometimes change whether and how often they pay for cancer screening tests. Check with your insurance plan to find out how often your insurance will cover a screening flexible sigmoidoscopy. If you don’t have insurance or your insurance won’t cover the procedure, call your local health department for help finding colorectal cancer screening tests.
How do I prepare for a flexible sigmoidoscopy?
To prepare for a flexible sigmoidoscopy, talk with your doctor about any health problems you have. Tell your doctor about any medicines, vitamins, and supplements you take.
You will also need to follow a special diet for a few days and clean out your bowel.
Follow a special diet
A health care professional will give you written instructions to follow at home before the procedure. The instructions will help you prepare for the procedure so that little or no stool remains in your large intestine. Stool inside your large intestine can prevent your doctor from clearly seeing the lining.
You may need to avoid dairy and foods that have a lot of fiber—such as whole grains, raw vegetables, beans, and nuts and seeds—several days before the procedure.
You may also need to follow a clear-liquid diet for a day or more before the procedure. The written instructions you receive will tell you when to start and stop the clear-liquid diet.
Clear liquids do not contain pulp, solids, or cream. Your doctor may also recommend avoiding red- and purple-colored drinks or gelatin. In most cases, you may drink or eat
- fat-free bouillon or broth
- gelatin in flavors such as lemon, lime, or orange
- plain coffee or tea, without cream or milk
- sports drinks in flavors such as lemon, lime, or orange
- fruit juice with no pulp, such as apple or white grape—avoid orange juice, pineapple juice, and other cloudy juices
- water
 Your doctor will give you specific instructions about how to prepare for the procedure.
Your doctor will give you specific instructions about how to prepare for the procedure.
Clean out your bowel
Flexible sigmoidoscopy often requires less bowel prep than colonoscopy. Your doctor will help you find the best bowel prep for you. You may also get written bowel prep instructions.
Different bowel preps may contain different combinations of enemas or laxatives. Some people will drink a large amount of liquid laxative over a scheduled period of time—most often, the night before and the morning of the procedure.
The bowel prep will cause diarrhea, so you should stay close to a bathroom. This part of the bowel prep can be challenging, but it’s important to finish the prep completely. Call a health care professional if you have side effects that keep you from finishing the prep.
How do doctors perform a flexible sigmoidoscopy?
A doctor performs a flexible sigmoidoscopy during an office visit or at a hospital or an outpatient center. The procedure usually takes about 10 to 20 minutes.3 You typically do not need sedatives or anesthesia.
During the procedure, you will lie on your left side while the doctor inserts a sigmoidoscope through your anus and into your rectum and lower colon. The scope inflates your colon with air for a better view. You may feel pressure or cramping during the procedure. The camera sends a video image to a monitor, allowing the doctor to examine the lining of your lower colon and rectum.
The doctor may ask you to move several times on the table to adjust the scope for better viewing. Once the scope reaches your transverse colon, the doctor slowly removes the scope and examines the lining of your lower colon again.
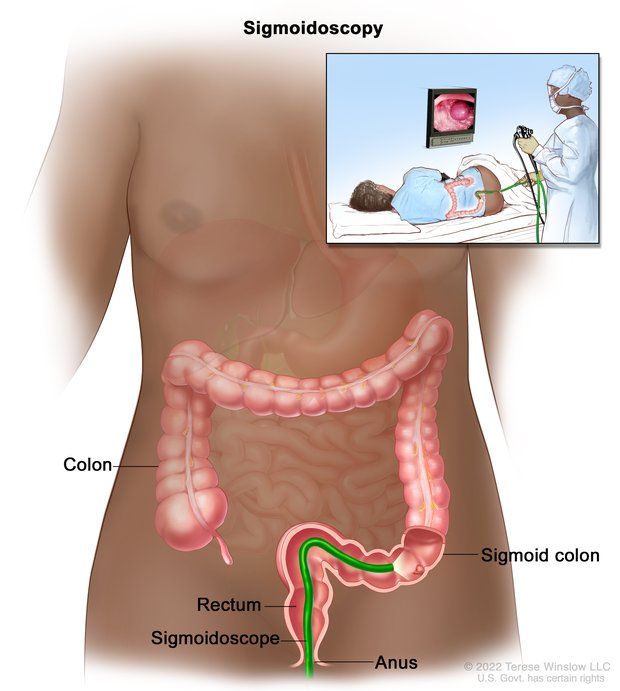 For the procedure, you’ll lie on your left side while the doctor inserts a sigmoidoscope through your anus and into your rectum and lower colon.
For the procedure, you’ll lie on your left side while the doctor inserts a sigmoidoscope through your anus and into your rectum and lower colon.
During the procedure, the doctor may remove polyps and send them to a lab for testing. You will not feel the polyp removal. Colon polyps are common in adults and are harmless in most cases. However, most colon cancers begin as a polyp, so removing polyps early may help prevent cancer.
If your doctor finds abnormal tissue, they may perform a biopsy. You won’t feel the biopsy.
You may need to return for a colonoscopy if your doctor finds polyps or other abnormal tissue during a flexible sigmoidoscopy.
What should I expect after a flexible sigmoidoscopy?
After a flexible sigmoidoscopy, you may feel cramping or bloating in your abdomen. You can typically return to your normal diet and activities right away if you didn’t receive a sedative or anesthesia.
If the doctor removed polyps or performed a biopsy, you may have light bleeding from your anus. This bleeding is normal.
Your doctor may share what they found during the procedure with you right away. If your doctor performed a biopsy, a pathologist will examine the biopsy tissue. Results take a few days or longer to come back. A health care professional will call you or schedule an appointment to go over the results.
What are the risks of a flexible sigmoidoscopy?
The risks of a flexible sigmoidoscopy include
- bleeding
- perforation of the colon
- severe pain in your abdomen
Bleeding and perforation are the most common complications from flexible sigmoidoscopy, but these are rare. A study of screening flexible sigmoidoscopies found that perforation occurs in about 1 out of every 50,000 procedures.4 Bleeding occurs in about 1 out of every 20,000 procedures.4 Most cases of bleeding occur in patients who have polyps removed.
The doctor can treat bleeding that happens during the flexible sigmoidoscopy right away. However, you may have delayed bleeding several days after the procedure. If you experience delayed bleeding, your doctor may diagnose and treat it with a colonoscopy or second flexible sigmoidoscopy.
The doctor may need to treat perforation with surgery.
References
This content is provided as a service of the National Institute of Diabetes and Digestive and Kidney Diseases
(NIDDK), part of the National Institutes of Health. NIDDK translates and disseminates research findings to increase knowledge and understanding about health and disease among patients, health professionals, and the public. Content produced by NIDDK is carefully reviewed by NIDDK scientists and other experts.
NIDDK would like to thank:
Michael B. Wallace, M.D., Mayo Clinic

