Alagille Syndrome
Return to Overview PageDefinition & Facts
In this section:
- What is Alagille syndrome?
- How common is Alagille syndrome?
- Who is more likely to have Alagille syndrome?
- What are the complications of Alagille syndrome?
What is Alagille syndrome?
Alagille syndrome is a genetic disorder that may affect many different parts of the body, including the liver, heart, eyes, face, skeleton, blood vessels, and kidneys.
A person with Alagille syndrome has fewer than the normal number of small bile ducts inside the liver. Bile ducts carry bile from the liver to the gallbladder for storage and then to the first part of the small intestine, also called the duodenum, for use in digestion. With fewer small bile ducts, less bile flows out of the liver. This condition is called cholestasis. As bile builds up in the liver, it may cause liver damage.
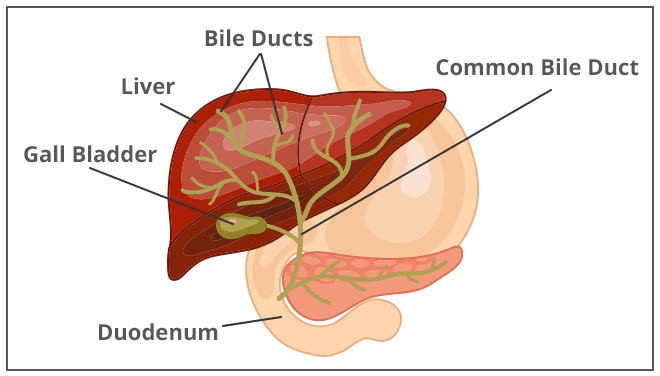 Bile ducts are tubes that carry bile from the liver to the gallbladder and the duodenum.
Bile ducts are tubes that carry bile from the liver to the gallbladder and the duodenum.
How common is Alagille syndrome?
About 1 in every 30,000 babies is born with Alagille syndrome.1
Who is more likely to have Alagille syndrome?
The gene mutation that causes Alagille syndrome can be passed from parent to child. Children who have one parent with Alagille syndrome have a 50 percent chance of inheriting the gene and having the disease.2
However, at least half—50 to 70 percent—of people with Alagille syndrome do not have a parent with the disease.3 In these cases, the disease is caused by a new gene mutation that is not inherited from a parent.
The liver signs and symptoms of Alagille syndrome usually appear shortly after birth or in early infancy. For this reason, Alagille syndrome is often diagnosed in children younger than age 1.4
What are the complications of Alagille syndrome?
Alagille syndrome can lead to complications that affect the liver and other parts of the body. Alagille syndrome varies greatly from person to person. In different people, the disease may affect different organs. The disease may also affect organs more seriously in some people than in others. Many people with Alagille syndrome have only mild symptoms and can lead normal lives with normal life expectancy. However, others have severe and even life-threatening complications such as liver failure, serious heart defects, and bleeding or stroke due to blood vessel problems.
Liver complications
In Alagille syndrome, less bile flows out of the liver, and the buildup of bile in the liver may cause liver damage.
Some young children with Alagille syndrome have a severe buildup of bile in the liver. In about half of these children, the flow of bile out of the liver improves by age 5. In the other half, the buildup of bile in the liver gets worse and leads to complications.5
Liver complications of Alagille syndrome may include
- cirrhosis, in which scar tissue replaces healthy liver tissue and prevents the liver from working normally. As cirrhosis gets worse, the liver begins to fail.
- portal hypertension, which occurs when scar tissue partly blocks the flow of blood through the liver, increasing pressure in the portal vein.
- liver failure, a condition in which the liver is badly damaged and stops working. Liver failure may require a liver transplant.
- liver cancer. Alagille syndrome increases the risk for liver cancer.
Other complications
Alagille syndrome may cause complications in other parts of the body, such as
- serious heart defects, such as tetralogy of Fallot, which require treatment with surgery
- narrowing and weakness in the blood vessels in the brain that may lead to bleeding and stroke
- problems with growth, delayed puberty, or failure to thrive
- bone problems, such as osteoporosis or frequent broken bones
References
Symptoms & Causes
What are the signs and symptoms of Alagille syndrome?
The most common signs and symptoms of Alagille syndrome are caused by less bile flowing out of the liver. Alagille syndrome may also affect other parts of the body, such as the heart, eyes, face, skeleton, blood vessels, and kidneys.
The signs and symptoms of Alagille syndrome vary, even among people in the same family. Some people with Alagille syndrome may have mild symptoms or may not know they have the disease. Others may have more severe symptoms, health problems, and complications.
Liver signs and symptoms
In Alagille syndrome, the reduced flow of bile out of the liver may lead to the following signs and symptoms
- severe itchiness of the skin, called pruritus
- yellowish color of the whites of the eyes and skin, called jaundice
- darkening of the color of urine and lightening of the color of stools
- fatty deposits that appear as yellow bumps on the skin, called xanthomas
- loose, greasy, bad-smelling stools, a sign that less bile is reaching the small intestine to help digest fats
- an enlarged liver or spleen, which a doctor may notice during a physical exam or imaging tests
These may be the first signs of Alagille syndrome and often appear in the first year of life.6 While Alagille syndrome commonly affects the liver, a small number of people with the disease have no signs or symptoms of reduced bile flow or liver disease.
Other signs and health problems
Alagille syndrome can affect many other parts of the body. Doctors may look for the following signs of the disease
- poor growth and energy, caused by the liver problems and other problems
- heart problems such as heart murmur and heart defects that are present at birth
- eye defects such as white or gray-white rings on the corneas, called posterior embryotoxon, which does not affect vision
- facial features such as a wide forehead and a pointed chin and nose
- bones of the skeleton that have an abnormal shape, such as bones in the spine shaped like butterflies, called butterfly vertebrae, which rarely cause problems
- narrowing and weakness in the walls of blood vessels, especially those in the head and neck
- kidney problems, including kidney dysplasia, renal tubular acidosis, and vesicoureteral reflux
What causes Alagille syndrome?
Gene mutations cause Alagille syndrome. Mutations of a gene called JAG1 cause most cases of Alagille syndrome. Mutations of a gene called NOTCH2 cause 1 to 2 percent of cases of Alagille syndrome.7
In at least half—50 to 70 percent—of people with Alagille syndrome, the disease is caused by a new gene mutation, meaning that the gene mutation was not inherited from a parent.7
In the remainder of people who have Alagille syndrome, the gene mutation for the disease is inherited from a parent. Alagille syndrome is an autosomal dominant disease, meaning that a child can get Alagille syndrome by inheriting a gene mutation from only one parent. Children who have one parent with Alagille syndrome have a 50 percent chance of inheriting the gene mutation and having the disease.8
References
Diagnosis
How do doctors diagnose Alagille syndrome?
Doctors diagnose Alagille syndrome based on signs and symptoms, medical and family history, a physical exam, an eye exam, and medical tests. Doctors may diagnose Alagille syndrome if a person has signs, symptoms, or health problems of the disease in three or more of the following areas
- liver
- heart
- eyes
- face
- skeleton
- blood vessels
- kidneys
Doctors may also diagnose Alagille syndrome if a person has signs, symptoms, or health problems in two of the above areas and also has a family member with Alagille syndrome.
Alagille syndrome can be difficult to diagnose because the signs and symptoms vary.
Medical and family history
The doctor will ask about a patient’s medical history and signs or symptoms, such as a yellowish color of the whites of the eyes and skin or changes in stool color. The doctor will also ask about the patient’s family history, including the history of liver diseases and other health problems.
Physical exam
During a physical exam, the doctor will check for signs of Alagille syndrome such as
- scratch marks on the skin from scratching the itching
- yellowish color of the whites of the eyes and skin
- fatty deposits that appear as yellow bumps on the skin
- enlargement of the liver or spleen
- facial features such as a wide forehead and a pointed chin and nose
- a heart murmur, which a doctor may hear with a stethoscope
Eye exam
During a slit-lamp exam, a doctor will use a special light to look for eye defects, such as a white or gray-white ring on the cornea.

What tests do doctors use to diagnose Alagille syndrome
Doctors may use blood tests, genetic tests, imaging tests, and liver biopsy to check for signs of Alagille syndrome and health problems related to this disease.
Blood tests
The doctor may order one or more blood tests to help diagnose Alagille syndrome. A health care professional will take blood samples and send the samples to a lab.
Blood tests may include
- liver function tests, which show how well the liver is working and may show signs of Alagille syndrome or other liver problems
- tests that check the levels of cholesterol and triglycerides, which are often higher than normal in people who have Alagille syndrome
- tests that check the levels of fat-soluble vitamins, which are often lower than normal in people who have Alagille syndrome
Genetic testing and counseling
The doctor may recommend genetic testing for gene mutations that cause Alagille syndrome. Genetic testing for these mutations is now widely available and increasingly reliable.
A health care professional will take a blood sample, which will be tested for gene mutations in a special lab. If a gene mutation for Alagille syndrome is found, a doctor may recommend testing the patient’s parents or other family members for the same mutation.
If you or your child have, or might have, Alagille syndrome and are considering genetic testing, you and your family may want to consider genetic counseling. Genetic counseling may be useful when you’re deciding whether to have genetic testing and again later when test results are available. Genetic counseling can help you and your family understand how test results may affect your lives.
Urinalysis
A urine sample is collected in a special container at a doctor’s office or at a lab. A health care professional will test the sample. Doctors may use urinalysis to check for signs of kidney problems related to Alagille syndrome or to rule out other health problems.
Imaging tests
To check for signs and health problems related to Alagille syndrome, doctors may order imaging tests. Imaging tests that doctors use to check for problems with the liver and biliary tract include
- ultrasound, which uses a device called a transducer, which bounces safe, painless sound waves off organs to create images of their structure.
- cholangiography, which is an x-ray of the bile ducts. Cholangiography may be performed during surgery or during a procedure called endoscopic retrograde cholangiopancreatography (ERCP).
- magnetic resonance cholangiopancreatography (MRCP), which uses a magnetic resonance imaging (MRI) machine to create pictures of the bile ducts and pancreatic ducts without x-rays or the need for a special procedure such as surgery or ERCP.
- hepatobiliary scan, which uses a small amount of safe radioactive material to create an image of the bile ducts.
Doctors may also order imaging tests to look for signs or health problems in other parts of the body. These tests may include
- ultrasound to check for kidney problems
- x-ray exam to check for skeletal defects
- echocardiogram, which uses sound waves to create pictures of the heart, to check for congenital heart defects
- magnetic resonance angiography, a type of MRI, to check for blood vessel problems
Liver biopsy
Doctors may order a liver biopsy if the results of other exams and test don’t confirm or rule out a diagnosis of Alagille syndrome.
During a liver biopsy, a doctor will take small pieces of tissue from your liver. A pathologist will examine the tissue under a microscope to look for features of specific liver diseases, such as Alagille syndrome, and check for liver damage and cirrhosis.
Treatment
How do doctors treat Alagille syndrome?
Doctors may refer people with Alagille syndrome to a hepatologist, a doctor who specializes in liver diseases, to treat liver symptoms and complications. Doctors may also refer patients to specialists who focus on other parts of the body, such as the heart, blood vessels, or kidneys.
Doctors may also recommend changes in diet and nutrition.
Liver symptoms
Doctors may prescribe ursodiol (Actigall, Urso) to improve the flow of bile from the liver to the small intestine. This medicine may help relieve severe itchy skin and reduce fatty deposits that appear as yellow bumps on the skin.
To help treat itchy skin, doctors may prescribe medicines such as cholestyramine, rifampin, naltrexone, or antihistamines. Doctors may also recommend using skin moisturizers, keeping baths and showers short, and trimming fingernails to prevent skin damage from scratching.
 Doctors may prescribe medicines to treat symptoms such as severe itchy skin.
Doctors may prescribe medicines to treat symptoms such as severe itchy skin.
In some cases, liver symptoms may be severe. For example, itchy skin may disturb sleep and affect everyday activities. The size and number of fatty deposits may change appearance or affect vision, eating, or movement. If these severe symptoms don’t improve with medicine, doctors may recommend operations such as
- partial external biliary diversion (PEBD). In PEBD, surgeons remove part of the small intestine and use it to connect the gallbladder to an opening in the abdomen called a stoma. Bile leaves the body through the stoma and is collected in a pouch.
- liver transplant. A doctor may recommend a liver transplant if severe itchy skin and fatty deposits don’t respond to other treatments.
If liver problems lead to enlargement of the spleen, doctors may recommend avoiding contact sports to prevent spleen injury.
Other signs and health problems
Doctors who specialize in the heart, blood vessels, or kidneys may prescribe medicines or recommend surgeries to treat health problems and prevent complications.
Some signs of Alagille syndrome typically don’t cause health problems or require treatment. Examples include bones in the spine shaped like butterflies, called butterfly vertebrae, and white or gray-white rings on the corneas, called posterior embryotoxon.
How do doctors treat the complications of Alagille syndrome?
Liver complications
If Alagille syndrome leads to cirrhosis and portal hypertension, doctors can treat related health problems and complications with medicines, surgery, and other medical procedures.
If cirrhosis leads to liver failure, a liver transplant may be needed. People with Alagille syndrome who have other severe health problems, such as serious heart defects, may not be good candidates for a liver transplant. In some cases, doctors may be able to correct other health problems before a liver transplant.
People who have Alagille syndrome have an increased chance of developing liver cancer. A doctor may order blood tests and an ultrasound or other types of imaging tests to check for liver cancer.
Other complications
Doctors may treat serious heart defects and blood vessel problems with surgery.
Doctors may recommend changes in diet and nutrition to treat or prevent bone problems, problems with growth, delayed puberty, or failure to thrive.
Can I prevent Alagille syndrome?
Experts have not yet found a way to prevent Alagille syndrome. People with Alagille syndrome should see their doctors regularly to help manage symptoms, health problems, and complications. Doctors may be able to prevent some complications or prevent complications from getting worse.
Eating, Diet, & Nutrition
How does Alagille syndrome affect nutrition?
In Alagille syndrome, the reduced flow of bile to the small intestine may cause problems with digesting fats and absorbing fat-soluble vitamins such as vitamins A, D, E, and K. These problems may cause malnutrition and play a part in causing complications such as bone problems, growth problems, delayed puberty, or failure to thrive.
What should people who have Alagille syndrome eat?
Getting enough nutrients is important for people who have Alagille syndrome, especially infants and children. Getting enough nutrients can help a child with Alagille syndrome grow as much as possible. If you or your child has Alagille syndrome, talk with a doctor or dietitian about a healthy eating plan.
Doctors and dietitians may recommend
- a high-calorie diet that contains carbohydrates and fats called medium-chain triglycerides (MCTs), which are easier for people with Alagille syndrome to digest
- a special formula for infants that contains MCTs
- regular checks of weight and height, the measures of growth and development during childhood
- regular blood tests to check vitamin levels and separate supplements of fat-soluble vitamins A, D, E, and K and other nutrients as needed
In some cases, children with Alagille syndrome can’t eat enough food to get the energy needed for growth. A doctor may recommend using a feeding tube to carry nutrients directly to the child’s stomach. The feeding tube may be a nasogastric tube, which is inserted through the nose, or a gastrostomy tube, which is inserted through a small surgical cut in the abdomen.
 Getting enough nutrients is important for people who have Alagille syndrome, especially infants and children.
Getting enough nutrients is important for people who have Alagille syndrome, especially infants and children.
What should people who have Alagille syndrome avoid eating?
People who have Alagille syndrome should talk with their doctor before drinking alcohol. Doctors may recommend not drinking alcohol if Alagille syndrome is causing liver problems.
Clinical Trials
The National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) and other components of the National Institutes of Health (NIH) conduct and support research into many diseases and conditions, including liver diseases.
What are clinical trials for Alagille syndrome?
Clinical trials—and other types of clinical studies—are part of medical research and involve people like you. When you volunteer to take part in a clinical study, you help doctors and researchers learn more about disease and improve health care for people in the future.
Researchers are studying many aspects of Alagille syndrome, such as how the disease progresses over time. Find out if clinical studies are right for you.
Watch a video of NIDDK Director Dr. Griffin P. Rodgers explaining the importance of participating in clinical trials.
What clinical studies for Alagille syndrome are looking for participants?
You can view a filtered list of clinical studies on Alagille syndrome that are federally funded, open, and recruiting at ClinicalTrials.gov. You can expand or narrow the list to include clinical studies from industry, universities, and individuals; however, the NIH does not review these studies and cannot ensure they are safe. Always talk with your health care provider before you participate in a clinical study.
What have we learned about Alagille syndrome from NIDDK-funded research?
The NIDDK has supported many research projects to learn more about Alagille syndrome. For example, the NIDDK supports the Childhood Liver Disease Research Network (ChiLDReN), which studies rare liver diseases that affect children, including Alagille syndrome. ChiLDReN researchers have made discoveries about
- how Alagille syndrome affects children’s health and quality of life
- the gene mutations that cause Alagille syndrome
- gene mutations that might affect the severity of the disease
This content is provided as a service of the National Institute of Diabetes and Digestive and Kidney Diseases
(NIDDK), part of the National Institutes of Health. NIDDK translates and disseminates research findings to increase knowledge and understanding about health and disease among patients, health professionals, and the public. Content produced by NIDDK is carefully reviewed by NIDDK scientists and other experts.
The NIDDK would like to thank:
David A. Piccoli, M.D., The Children's Hospital of Philadelphia
