Peptic Ulcers (Stomach or Duodenal Ulcers)
Return to Overview PageDefinition & Facts
In this section:
- What is a peptic ulcer?
- How common are peptic ulcers?
- Who is more likely to develop peptic ulcers?
- What are the complications of peptic ulcers?
What is a peptic ulcer?
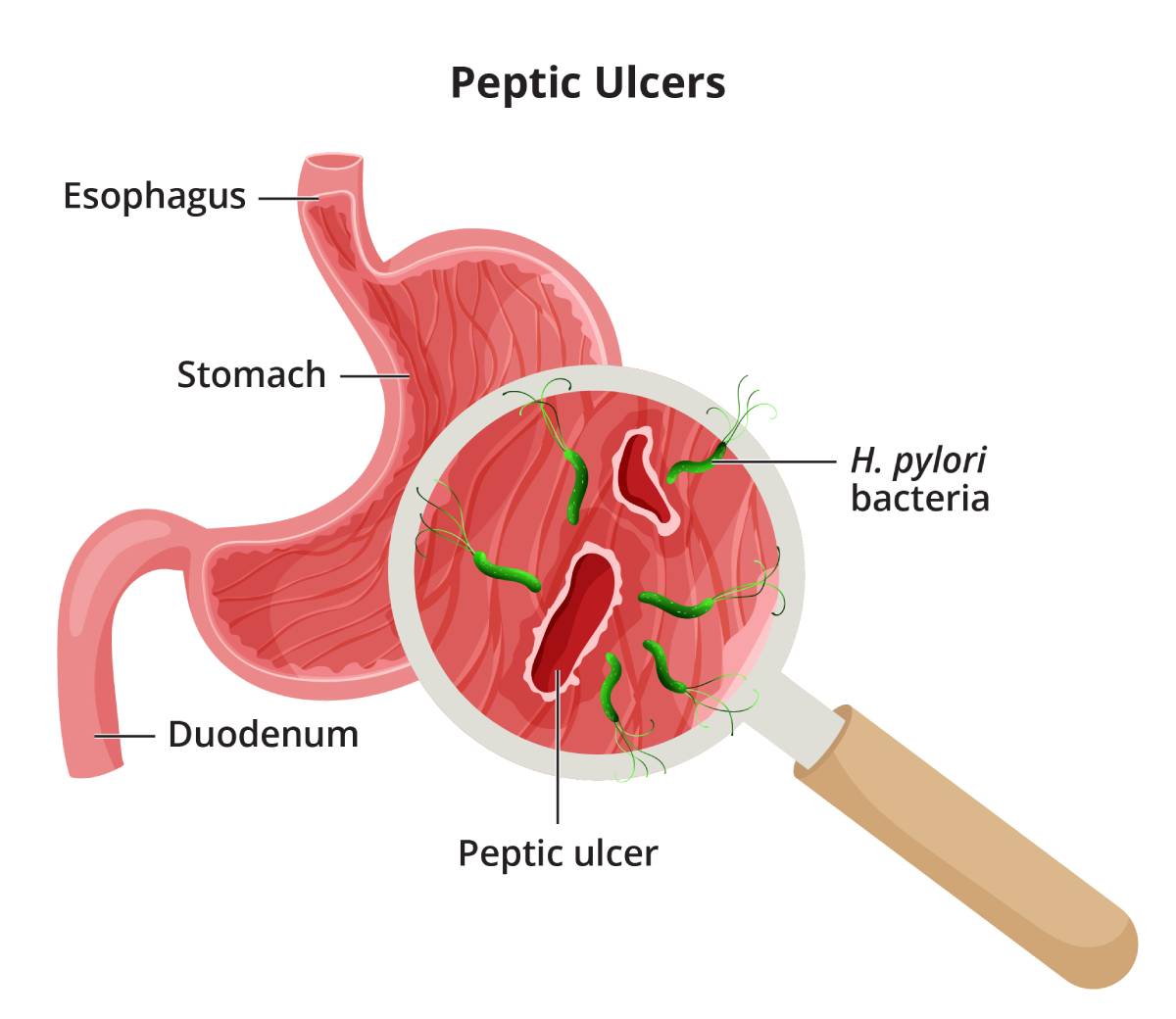
A peptic ulcer is a sore on the lining of your stomach or duodenum.
Do peptic ulcers have other names?
Peptic ulcers are sometimes called stomach ulcers, duodenal ulcers, or peptic ulcer disease.
How common are peptic ulcers?
Researchers estimate about 1% to 6% of people in the United States have peptic ulcers.1
Who is more likely to develop peptic ulcers?
People are more likely to develop peptic ulcers if they are
- infected with the bacteria Helicobacter pylori (H. pylori)
- taking nonsteroidal anti-inflammatory drugs (NSAIDs), such as aspirin, ibuprofen, and naproxen
H. pylori infection and taking NSAIDs are the two most common causes of peptic ulcers.
People also are more likely to develop peptic ulcers if they
- are older adults
- had a peptic ulcer before
- smoke
What are the complications of peptic ulcers?
Peptic ulcers can lead to complications such as
- bleeding in your stomach or duodenum
- a perforation, or hole, in the wall of your stomach or duodenum, which can lead to peritonitis, an infection of the lining of the abdominal cavity
- penetration of the ulcer through the stomach or duodenum and into another nearby organ
- a blockage that can stop food from moving from your stomach into your duodenum
Reference
Symptoms & Causes
What are the symptoms of a peptic ulcer?
Peptic ulcers may cause symptoms of indigestion. Common symptoms include
- pain or discomfort in the upper part of your abdomen, anywhere between your belly button and breastbone
- feeling full too soon while eating a meal
- feeling uncomfortably full after eating a meal
- nausea and vomiting
- bloating
- belching
 Abdominal pain is the most common symptom of a peptic ulcer.
Abdominal pain is the most common symptom of a peptic ulcer.Abdominal pain is the most common symptom of a peptic ulcer. The pain may be dull or burning and may come and go over time. For some people, the pain may occur when the stomach is empty or at night, and it may go away for a short time after they eat. For other people, eating may make the pain worse.
Many people who have peptic ulcers don’t have any symptoms. They may not develop symptoms until an ulcer leads to complications.
You should call or see your doctor right away if you have symptoms that could be caused by a complication. These symptoms include
- black or tarry stool, or red or maroon blood mixed with your stool
- red blood in your vomit or vomit that looks like coffee grounds
- sudden, sharp, or severe abdominal pain that doesn’t go away
- feeling dizzy or fainting
- a rapid pulse or other symptoms of shock
- a change in or worsening of your peptic ulcer symptoms
What causes peptic ulcers?
The most common causes of peptic ulcers are Helicobacter pylori (H. pylori) infection and nonsteroidal anti-inflammatory drugs (NSAIDs). Other causes of peptic ulcers are uncommon or rare.
People with certain risk factors are more likely to develop ulcers.
H. pylori
H. pylori infection is a common cause of peptic ulcers. Researchers are still studying how people become infected with H. pylori bacteria. The bacteria may spread from person to person through contact with an infected person’s vomit, stool, or saliva. Food or water contaminated with an infected person’s vomit, stool, or saliva may also spread the bacteria from person to person.
NSAIDs
Taking NSAIDs—such as aspirin, ibuprofen, and naproxen—is another common cause of peptic ulcers. NSAIDs relieve pain, but they also make the stomach lining more prone to damage and ulcers. Some types of NSAIDs are more likely to cause ulcers than others.
You have a higher chance of developing a peptic ulcer due to NSAIDs if you take
- NSAIDs for a long time
- a type of NSAID that is more likely to cause an ulcer
- high doses of an NSAID or more than one NSAID
- NSAIDs along with other medicines that increase the risk for ulcers
- NSAIDs and you are also infected with H. pylori
Other causes
Less common causes of peptic ulcers include
- infections caused by certain viruses, fungi, or bacteria other than H. pylori
- medicines that increase the risk of developing ulcers, including corticosteroids, medicines used to treat low bone mass, and some antidepressants, especially when you take these medicines with NSAIDs
- surgery or medical procedures that affect the stomach or duodenum
Less common causes of peptic ulcers also include certain diseases and health conditions, such as
- diseases that can affect the stomach, such as cancer or Crohn’s disease
- injury, blockage, or lack of blood flow that affects the stomach or duodenum
- life-threatening health conditions that require critical care
- severe chronic diseases, such as cirrhosis or chronic obstructive pulmonary disease
- Zollinger-Ellison syndrome, a condition that occurs when one or more tumors—called gastrinomas—cause your stomach to make too much acid
In rare cases, doctors can’t find the cause of peptic ulcers. Doctors may call ulcers with unknown causes idiopathic peptic ulcers.
Diagnosis
How do doctors diagnose a peptic ulcer?
Your doctor may ask you about your medical and family history, perform a physical exam, and order tests to diagnose a peptic ulcer, find its cause, and check for complications.
Medical and family history
To help diagnose peptic ulcers and check for factors that cause ulcers, your doctor will take a medical and family history. Your doctor may ask about
- your symptoms
- your medical history, including any past peptic ulcers or Helicobacter pylori (H. pylori) infections
- medicines you take, especially nonsteroidal anti-inflammatory drugs (NSAIDs)
- your family history of peptic ulcers, H. pylori infection, or cancer in the digestive tract
 To help diagnose a peptic ulcer, your doctor will take a medical and family history.
To help diagnose a peptic ulcer, your doctor will take a medical and family history.
Physical exam
A physical exam may help a doctor diagnose peptic ulcers or ulcer complications. During a physical exam, a doctor most often
- checks for swelling in your abdomen
- listens to sounds within your abdomen using a stethoscope
- taps on your abdomen checking for tenderness or pain
What tests do doctors use to diagnose peptic ulcers?
Doctors may order medical tests to help diagnose peptic ulcers, find the cause, and check for complications.
Blood test
Doctors may use blood tests to check for signs of H. pylori infection or complications of peptic ulcers. For a blood test, a health care professional will take a blood sample from you and send the sample to a lab.
Urea breath test
Doctors may use a urea breath test to check for H. pylori infection. For the test, you will swallow a capsule, liquid, or pudding that contains urea “labeled” with a special carbon atom. If H. pylori is present, the bacteria will convert the urea into carbon dioxide. After a few minutes, you will breathe into a container, exhaling carbon dioxide.
A health care professional will test your exhaled breath. If the test detects the labeled carbon atoms, the health care professional will confirm an H. pylori infection in your digestive tract.
Stool test
Doctors may use stool tests to check for H. pylori infection. Your doctor will give you a container for catching and holding a stool sample. You will receive instructions on where to send or take the kit for testing.
Upper gastrointestinal (GI) endoscopy and biopsy
Doctors may order an upper GI endoscopy to confirm the diagnosis of a peptic ulcer and try to find its cause.
For an upper GI endoscopy, a doctor uses an endoscope—a flexible tube with a camera—to see the lining of your upper GI tract, including your esophagus, stomach, and duodenum. During upper GI endoscopy, a doctor obtains biopsies by passing an instrument through the endoscope to take small pieces of tissue from your stomach lining. A pathologist will examine the tissue under a microscope.
Upper GI series
In some cases, doctors may order an upper GI series to help diagnose peptic ulcers or ulcer complications. Upper GI series uses x-rays and a chalky liquid you swallow called barium to view your upper GI tract.
Treatment
How do doctors treat peptic ulcers?
To treat peptic ulcers, doctors typically recommend medicines to help the ulcer heal. They also look for the cause of ulcers and treat or manage the cause. Talk with your doctor about the best treatment plan for you.
Healing peptic ulcers
Medicines that doctors recommend or prescribe to treat peptic ulcers include
- proton pump inhibitors (PPIs)
- H2 blockers
- other medicines
Treating the causes of peptic ulcers
Doctors treat the underlying causes of peptic ulcers to help the ulcers heal and prevent them from coming back.
Helicobacter pylori (H. pylori) infection
Doctors treat H. pylori infection with a combination of medicines. These medicines most often include
- two or more antibiotics
- a PPI
- in some cases, bismuth subsalicylate
Your doctor may avoid prescribing antibiotics you’ve taken in the past because the H. pylori bacteria may have developed antibiotic resistance to those antibiotics.
If you are given medicines, take all doses exactly as your doctor prescribes. If you stop taking your medicine early, some bacteria may survive and persist in your stomach. In other words,
H. pylori bacteria may develop antibiotic resistance.
To find out if the medicines worked, your health care professional may recommend testing you for H. pylori at least 4 weeks after you’ve finished taking the antibiotics.2 If you still have an
H. pylori infection, your doctor may prescribe a different combination of antibiotics and other medicines to treat the infection. Making sure that all of the H. pylori bacteria have been killed is important.
Nonsteroidal anti-inflammatory drugs (NSAIDs)
 If you have a peptic ulcer caused by taking NSAIDs,
your doctor may recommend changing your medicines.
If you have a peptic ulcer caused by taking NSAIDs,
your doctor may recommend changing your medicines.If you have a peptic ulcer caused by taking NSAIDs, your doctor may recommend changing your medicines. Depending on the reason you have been taking NSAIDs, your doctor may suggest stopping NSAIDs, taking a different NSAID, taking a lower-dose NSAID, or taking a different medicine for pain.
If you need to keep taking NSAIDs, your doctor may recommend you also take a PPI.
Other causes
If your peptic ulcers aren’t caused by H. pylori infection or NSAIDs, doctors will check for uncommon causes. Depending on the cause, doctors may recommend additional treatments.
What if an ulcer doesn’t heal or comes back after treatment?
Taking medicines and treating the underlying cause heals most ulcers. However, if your ulcer doesn’t heal or comes back after treatment, your doctor may
- check for and treat any factors that could be causing the ulcer, such as an H. pylori infection.
- recommend you quit smoking, if you smoke. Smoking can slow ulcer healing.
- recommend or prescribe more medicines to help heal the ulcer.
- recommend an upper GI endoscopy to obtain biopsies.
In rare cases, doctors may recommend surgery to treat peptic ulcers that don’t heal.
How do doctors treat the complications of peptic ulcers?
Doctors typically treat complications of peptic ulcers in a hospital. In addition to treating the ulcer, doctors may recommend medical procedures, such as an upper GI endoscopy, or surgery to treat ulcer complications.
How can I prevent peptic ulcers?
If you smoke, quitting smoking can lower your risk for peptic ulcers.
If your doctor thinks you have a high risk for developing peptic ulcers caused by taking NSAIDs, your doctor may recommend changes to lower your risk, such as
- changing the medicines you take, if possible. For example, your doctor may change the type of NSAIDs you take, lower the dose of NSAIDs, or prescribe NSAIDs for a shorter time.
- taking PPIs along with NSAIDs.
- testing for and treating H. pylori infection before you start taking long-term NSAIDs.
If you have a peptic ulcer, finding and treating the underlying cause, such as H. pylori infection, can help lower the chance of developing future ulcers.
Reference
Eating, Diet, & Nutrition
Can changes to my diet help prevent or treat a peptic ulcer?
Researchers have not found that diet and nutrition play an important role in causing, preventing, or treating peptic ulcers. Doctors do not recommend following a special diet or avoiding specific foods or drinks to prevent or treat ulcers.
If you smoke, quitting smoking can lower your risk for developing ulcers and help existing ulcers heal.
Clinical Trials
The NIDDK conducts and supports clinical trials in many diseases and conditions, including digestive diseases. The trials look to find new ways to prevent, detect, or treat disease and improve quality of life.
What are clinical trials for peptic ulcers?
Clinical trials—and other types of clinical studies—are part of medical research and involve people like you. When you volunteer to take part in a clinical study, you help doctors and researchers learn more about disease and improve health care for people in the future.
Researchers are studying many aspects of peptic ulcers, including
- new ways to diagnose peptic ulcers
- improved diagnostic tests and treatments for Helicobacter pylori (H. pylori) infection
- ways to prevent and treat peptic ulcer complications
Find out if clinical studies are right for you.
Watch a video of NIDDK Director Dr. Griffin P. Rodgers explaining the importance of participating in clinical trials.
What clinical studies for peptic ulcers are looking for participants?
You can view a filtered list of clinical studies on peptic ulcers that are federally funded, open, and recruiting at ClinicalTrials.gov. You can expand or narrow the list to include clinical studies from industry, universities, and individuals; however, the NIH does not review these studies and cannot ensure they are safe. Always talk with your health care provider before you participate in a clinical study.
This content is provided as a service of the National Institute of Diabetes and Digestive and Kidney Diseases
(NIDDK), part of the National Institutes of Health. NIDDK translates and disseminates research findings to increase knowledge and understanding about health and disease among patients, health professionals, and the public. Content produced by NIDDK is carefully reviewed by NIDDK scientists and other experts.
The NIDDK would like to thank:
Richard M. Peek, Jr., M.D., Vanderbilt University Medical Center