Polycystic Kidney Disease
Return to Overview PageWhat is PKD?
In this section:
- What are the types of PKD?
- How common is PKD?
- Who is more likely to have PKD?
- What causes PKD?
- What are the signs and symptoms of PKD?
- Can I prevent PKD?
- What can I do to slow down PKD?
Polycystic kidney disease (PKD) is a genetic disorder that causes many fluid-filled cysts to grow in your kidneys. Unlike the usually harmless simple kidney cysts that can form in the kidneys later in life, PKD cysts can change the shape of your kidneys, including making them much larger.
PKD is a form of chronic kidney disease (CKD) that reduces kidney function and may lead to kidney failure. PKD also can cause other complications, or problems, such as high blood pressure, cysts in the liver, and problems with blood vessels in your brain and heart.
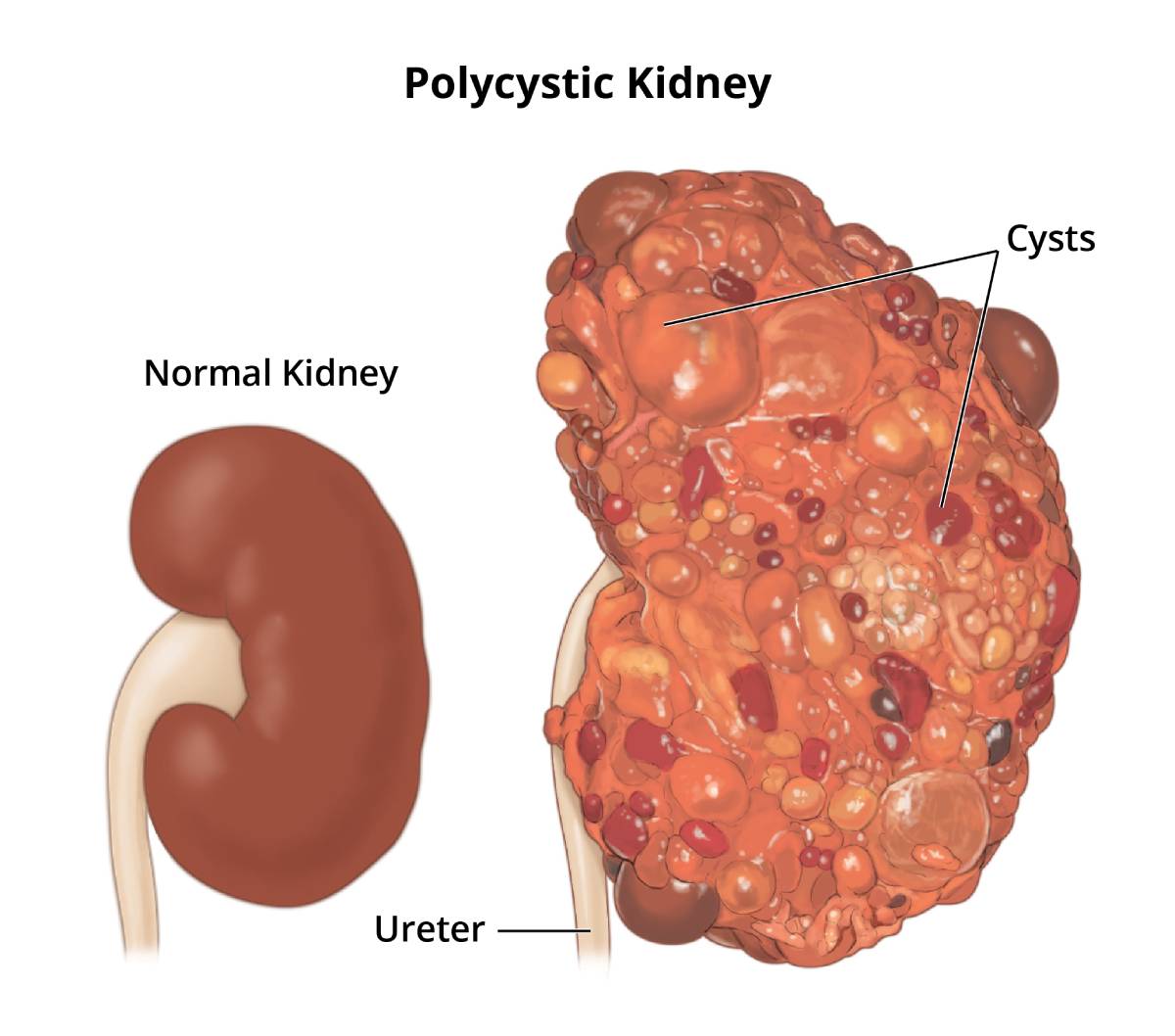 Polycystic kidney disease is a genetic disorder that causes many fluid-filled cysts to grow in your kidneys.
Polycystic kidney disease is a genetic disorder that causes many fluid-filled cysts to grow in your kidneys.
What are the types of PKD?
The two main types of PKD are
- autosomal dominant PKD (ADPKD), which is usually diagnosed in adulthood
- autosomal recessive PKD (ARPKD), which can be diagnosed in the womb or shortly after a baby is born
How common is PKD?
PKD is one of the most common genetic disorders. PKD affects about 500,000 people in the United States.1
ADPKD affects 1 in every 400 to 1,000 people in the world, and ARPKD affects 1 in 20,000 children.2,3
Who is more likely to have PKD?
PKD affects people of all ages, races, and ethnicities worldwide. The disorder occurs equally in women and men.
What causes PKD?
A gene mutation, or defect, causes PKD. In most PKD cases, a child got the gene mutation from a parent. In a small number of PKD cases, the gene mutation developed on its own, without either parent carrying a copy of the mutated gene. This type of mutation is called “spontaneous.” Read more about genes and genetic conditions.
What are the signs and symptoms of PKD?
The signs and symptoms of ADPKD, such as pain, high blood pressure, and kidney failure, are also PKD complications. In many cases, ADPKD does not cause signs or symptoms until your kidney cysts are a half inch or larger in size.
Early signs of ARPKD in the womb are larger-than-normal kidneys and a smaller-than-average size baby, a condition called growth failure. The early signs of ARPKD are also complications. However, some people with ARPKD do not develop signs or symptoms until later in childhood or even adulthood.
Can I prevent PKD?
Researchers have not yet found a way to prevent PKD. However, you may be able to slow PKD problems caused by high blood pressure, such as kidney damage. Aim for a blood pressure goal of less than 120/80. Work with a health care team to help manage your or your child’s PKD. The health care team will probably include a general practitioner and a nephrologist, a health care provider specializing in kidney health.
What can I do to slow down PKD?
The sooner you know you or your child has PKD, the sooner you can keep the condition from getting worse. Getting tested if you or your child are at risk for PKD can help you take early action.
You also can take steps to help delay or prevent kidney failure. Healthy lifestyle practices such as being active, reducing stress, and quitting smoking can help.
Make lifestyle changes
Be active for 30 minutes or more on most days. Regular physical activity can help you reduce stress, manage your weight, and control your blood pressure. If you are not active now, ask your health care provider about how much and what type of physical activity is right for you.
If you play contact sports, such as football or hockey, a health care provider should do a magnetic resonance imaging (MRI) test to see whether these sports are safe for you. Trauma to your body, especially to your back and sides, may cause kidney cysts to burst.
Lose weight. Being overweight makes your kidneys work harder. Losing weight helps protect your kidneys.
Aim for 7 to 8 hours of sleep each night. Getting enough sleep is important to your overall physical and mental health and can help you manage your blood pressure and blood glucose, or blood sugar.
Reduce stress. Long-term stress can raise your blood pressure and even lead to depression. Some of the steps you take to manage your PKD are also healthy ways to cope with stress. For example, getting enough physical activity and sleep helps reduce stress.
Quit smoking. Cigarette smoking can raise your blood pressure, making your kidney damage worse. Quitting smoking may help you meet your blood pressure goals, which is good for your kidneys and can lower your chances of having a heart attack or stroke. Quitting smoking is even more important for people with PKD who have aneurysms. An aneurysm is a bulge in the wall of a blood vessel. For tips on quitting, go to Smokefree.gov.

Change what you eat and drink
You may need to change what you eat and drink to help control your blood pressure and protect your kidneys. People with any kind of kidney disease, including PKD, should talk with a dietitian about which foods and drinks to include in their healthy eating plan and which may be harmful. Staying hydrated by drinking the right amount of fluid may help slow PKD’s progress toward kidney failure. Read more about what to eat or drink if you have PKD or are at risk for PKD.
Take blood pressure medicines
If lifestyle and diet changes don’t help control your blood pressure, a health care provider may prescribe one or more blood pressure medicines. Two types of blood pressure medicines, angiotensin-converting enzyme (ACE) inhibitors and angiotensin receptor blockers (ARBs), may slow kidney disease and delay kidney failure. The names of these medicines end in –pril or –sartan.
References
Autosomal Dominant PKD
In this section:
- What is autosomal dominant PKD?
- What are the most common complications of ADPKD?
- What are other complications of ADPKD?
- What are the signs and symptoms of ADPKD?
- How do health care providers diagnose ADPKD?
- How does my health care team treat the most common complications of ADPKD?
- How does ADPKD affect my day-to-day life?
What is autosomal dominant PKD?
Autosomal dominant polycystic kidney disease (ADPKD) is the most common form of PKD. ADPKD affects 1 in every 400 to 1,000 people and is the most common kidney disorder passed down through family members.4 Health care providers usually diagnose ADPKD between the ages of 30 and 50, when signs and symptoms start to appear, which is why it is sometimes called “adult PKD.”5
“Autosomal dominant” means you can get the PKD gene mutation, or defect, from only one parent. Researchers have found two different gene mutations that cause ADPKD. Most people with ADPKD have defects in the PKD1 gene, and 1 out of 6 or 1 out of 7 people with ADPKD have a defective PKD2 gene.6
Health care providers can diagnose people with PKD1 sooner because their symptoms appear sooner. People with PKD1 also usually progress more quickly to kidney failure than people with PKD2. How quickly ADPKD progresses also differs from person to person.
What are the most common complications of ADPKD?
Most people with ADPKD have pain, high blood pressure, and kidney failure at some point in their lives.
Pain
Pain is a common complication of ADPKD and is usually due to kidney or liver cysts. Pain also can be caused by
- kidney cyst infection
- bleeding or burst kidney cysts
- urinary tract infection
- kidney stones
- tissue stretching around the kidney due to cyst growth
High blood pressure
Almost all people with ADPKD who have kidney failure have high blood pressure. High blood pressure increases your chances of heart disease and stroke. High blood pressure can also damage your kidneys even more. Keep your blood pressure under control to help delay kidney damage.
Kidney failure
Kidney failure means your kidneys no longer work well enough to stay healthy. Untreated kidney failure can lead to coma and death. More than half of people with ADPKD progress to kidney failure by age 70.7
What are other complications of ADPKD?
ADPKD complications, or problems, can affect many systems in your body besides your kidneys. Researchers have not found a link between PKD and kidney cancer.
You may see some ADPKD complications right away. Other complications may not appear for many years, depending on whether you have the PKD1 or PKD2 gene. Also, ADPKD complications can vary from person to person, so you may not have all of these problems.
Vascular system problems
Abnormal heart valves. Abnormal heart valves can occur in some people with ADPKD. Abnormal heart valves can cause too little blood to flow into the aorta, the large artery that carries blood from the heart to the rest of your body. Abnormal heart valves in people with ADPKD rarely need to be replaced. However, you may need more tests if your health care provider detects a heart murmur.
Brain aneurysms. An aneurysm is a bulge in the wall of a blood vessel. Aneurysms in the brain might cause headaches that are severe or feel different from other headaches. See a health care provider even before you take over-the-counter pain medicines for severe headaches or headaches that won’t go away.
Brain aneurysms can break open and cause bleeding inside the skull. Large brain aneurysms are life threatening and need immediate medical treatment. If you have an aneurysm, stop smoking and control your blood pressure and lipids.
Digestive system problems
Liver cysts. Liver cysts, which are fluid-filled cysts on the liver, are the most common nonkidney complication of ADPKD. Liver cysts don’t usually cause symptoms in people under age 30, because liver cysts are normally small and few in number in the early stages of ADPKD. In rare cases, liver cysts can eventually reduce liver function. In the most severe cases, you may need a liver transplant.
Because the hormone estrogen may affect liver cyst growth, women are more likely to have liver cysts than men. The more pregnancies a woman with ADPKD has had, the more likely she will have liver cysts.7
Pancreatic cysts. PKD can also cause cysts in your pancreas. Pancreatic cysts rarely cause pancreatitis, which is inflammation, or swelling, of the pancreas.
Diverticula. Diverticula are small pouches, or sacs, that push through weak spots in your colon wall. Diverticula can cause diverticulosis. Diverticulosis can cause changes in your bowel movement patterns or pain in your abdomen.
Urinary tract problems
Urinary tract infections (UTIs). Kidney cysts can block urine flow through the kidneys so that urine stays in your urinary tract too long. When urine stays in your urinary tract too long, bacteria in your urine can cause a bladder infection or a kidney infection. A kidney infection can cause further damage to your kidneys by causing cysts to become infected.
Kidney stones. People with ADPKD sometimes have kidney stones. Kidney stones can block urine flow and cause infection and pain.
Reproductive problems
Although most women with PKD have normal pregnancies, women with PKD who have high blood pressure and decreased kidney function are more likely to have preeclampsia, or high blood pressure during pregnancy.
With preeclampsia, the fetus gets less oxygen and fewer nutrients. Women with preeclampsia should be followed closely by their health care provider during and after pregnancy. After delivery, preeclampsia goes away.
Many men with ADPKD have cysts on their seminal vesicles, which are glands in the male reproductive system that help produce semen. Seminal vesicle cysts rarely cause infertility.
People with PKD who are considering having children may want to discuss family planning concerns with a genetics counselor.
What are the signs and symptoms of ADPKD?
In many cases, ADPKD doesn’t cause signs or symptoms until cysts are a half inch or larger in size. For this reason, you should meet with a health care provider if you are at risk for PKD before your symptoms start.
The most common symptoms are pain in the back and sides, between the ribs and hips, and headaches. The pain can be short term or ongoing, mild or severe.
Hematuria, or blood in the urine, may be a sign of ADPKD. If you have hematuria, see a health care provider right away.
How do health care providers diagnose ADPKD?
Health care providers diagnose ADPKD using imaging tests and genetic testing. A health care provider can make a diagnosis based on these tests and your age, family history of PKD, and how many cysts you have.
The sooner a health care provider can diagnose ADPKD, the better your chances of delaying complications.
Imaging tests
A specially trained technician performs imaging tests in a health care provider’s office, an outpatient center, or a hospital. A radiologist reads the images. Adults usually don’t need anesthesia for these tests. However, a health care provider may give infants or children a sedative to help them fall asleep during the test.
Ultrasound. Ultrasound uses a device called a transducer that bounces safe, painless sound waves off your organs to create an image of their structure. An abdominal ultrasound can create images of your entire urinary tract or focus specifically on the kidneys. The images can show cysts in the kidneys.
Computed tomography (CT) scans. CT scans use a combination of x-rays and computer technology to create images of your urinary tract. For a CT scan of your urinary tract, a health care provider may give you an injection of contrast medium. Contrast medium is a dye or other substance that makes structures inside your body easier to see during imaging tests. You lie on a table that slides into a tunnel-shaped device that takes the x-rays. CT scans can show more detailed images of kidney cysts than ultrasound.
Magnetic resonance imaging (MRI). MRI machines use radio waves and magnets to produce detailed pictures of your body’s internal organs and soft tissues without using x-rays. An MRI may include an injection of contrast medium. With most MRI machines, you lie on a table that slides into a tunnel-shaped machine that may be open on each end or closed at one end. Some newer machines allow you to lie in a more open space. Health care providers use MRIs to measure kidney and cyst size and monitor kidney and cyst growth. Measuring kidney and cyst size and growth can help track the progress of PKD.
Genetic testing
Your health care provider may refer you to a geneticist if you are at risk for ADPKD. A geneticist is an expert in genes and diseases that are passed down through families. You will provide the geneticist with a blood or saliva sample, which will be tested in a special lab for the gene mutations that cause ADPKD. The genetic testing may take many days or weeks to complete.
A health care provider may also use genetic testing results to find out whether someone with a family history of PKD is likely to develop PKD in the future.
When to consider genetic counseling
If you are considering genetic testing, you and your family may want to talk with a genetics counselor as part of your health care team. Genetic counseling may be useful when you’re deciding whether to have genetic testing and again later when test results are available. Genetic counseling can help you and your family understand how test results may affect your lives.

How does my health care team treat the most common complications of ADPKD?
Although a cure doesn’t exist yet for ADPKD, treatment can help reduce your complications, which can help you live longer.
Manage pain
A health care provider needs to find the source of your pain before he or she can treat it. For example, if growing cysts are causing pain, the health care provider may first suggest over-the-counter (OTC) pain medicines such as aspirin or acetaminophen.
Always talk with a health care provider before taking any OTC medicines because some may be harmful to your kidneys. People with ADPKD have a higher risk for acute kidney injury (AKI), which is the sudden and temporary loss of kidney function. Sometimes AKI is caused by using OTC painkillers for a long time.
Depending on the size and number of cysts and whether medicine helps your pain, a health care provider may suggest surgery. Surgery to shrink cysts can help pain in your back and sides for a while. However, surgery does not slow PKD’s progress toward kidney failure.
Control your blood pressure
Controlling your blood pressure can slow the effects of ADPKD. Lifestyle changes and medicines can lower high blood pressure. Sometimes you can control blood pressure with healthy eating and regular physical activity alone.
Some health care providers will recommend blood pressure medicines called angiotensin-converting enzyme (ACE) inhibitors or angiotensin receptor blockers (ARBs).
Treat kidney failure
ADPKD can eventually cause your kidneys to fail. People with kidney failure must have dialysis or a kidney transplant to replace their kidney function.
The two forms of dialysis are hemodialysis and peritoneal dialysis. Hemodialysis uses a machine to circulate your blood through a filter outside the body. Peritoneal dialysis uses the lining of your abdomen to filter the blood inside the body.
A kidney transplant is surgery to place a healthy kidney from a donor into your body.
How does ADPKD affect my day-to-day life?
Managing PKD successfully will probably include several lifestyle changes, such as changes in your physical activity level and what you eat. Visiting with a health care team on a regular basis is an important part of your routine as you work to limit your kidney problems.
PKD is a costly disease to manage and treat, especially if health insurance doesn’t cover some or any of your costs. Financial help may be available from the Federal Government and other sources. Visit the Centers for Medicare & Medicaid Services website or talk with your health care team for more information.
Many people with PKD may find it hard, but not impossible, to get life insurance. Contact an insurance company that specializes in “impaired risk life insurance.”
References
Autosomal Recessive PKD
In this section:
- What is autosomal recessive PKD?
- What are the early signs of ARPKD?
- What are the complications of ARPKD?
- How do health care providers diagnose ARPKD?
- How do health care providers treat the complications of ARPKD?
What is autosomal recessive PKD?
Autosomal recessive polycystic kidney disease (ARPKD) is a rare genetic disorder that affects 1 in 20,000 children.8 A fetus or baby with ARPKD has fluid-filled kidney cysts that may make the kidneys too big, or enlarged. ARPKD can cause a child to have poor kidney function, even in the womb. ARPKD is sometimes called “infantile PKD” because health care providers can diagnose it so early in life.
Poor kidney function can cause breathing problems that can threaten the life of a fetus or baby. About 30 percent of newborns with ARPKD die within their first week of life.8 A baby with ARPKD who survives birth and the first few weeks of life has a good chance of surviving into adulthood. However, children or young adults with ARPKD will likely need medical treatment their whole life.
“Autosomal recessive” means that for a child to have this disorder, both parents must have and pass along the gene mutation. If only one parent carries the mutated gene, the child will not get the disorder, although the child may get the gene mutation. The child is a “carrier” of the disorder and can pass the gene mutation to the next generation.
How quickly ARPKD progresses to kidney failure is different for each child. The sooner a fetus is diagnosed in the womb, the better the child’s outlook. Getting good prenatal care is important for increasing a child’s survival rate. Working with a health care team as soon as possible can help parents manage their child’s PKD.

What are the early signs of ARPKD?
The early signs of ARPKD often appear during the first few months of life and in the womb. Early signs of ARPKD in the womb can cause serious health problems. For this reason, it is important for a woman who is at risk for passing PKD to her children to get prenatal care as soon as she learns she is pregnant.
Enlarged kidney. An early sign of ARPKD is an enlarged kidney. Enlarged kidneys put pressure on a fetus’ or child’s lungs, which can make lung growth and breathing harder. A health care provider can see enlarged kidneys in a fetus or an infant using ultrasound imaging, also called a sonogram.
Growth failure. Due to decreased kidney and lung function, children with ARPKD are usually smaller-than-average size, a condition called growth failure.
Low levels of amniotic fluid. Decreased kidney function can cause low levels of amniotic fluid in a mother’s womb. Low levels of amniotic fluid can cause breathing problems in the fetus.
Some people with ARPKD do not develop signs or symptoms until later in childhood, or even adulthood.
What are the complications of ARPKD?
Children with ARPKD who survive birth often have kidney and liver problems that can affect their breathing. Working with a health care team as soon as possible can help manage these complications.
Breathing problems. Babies with the most severe cases of ARPKD often die hours or days after birth because they cannot breathe well enough to live. Their lungs do not develop as they should in the womb.
Kidney failure. Children born with ARPKD often develop kidney failure before reaching adulthood.
Liver problems. Liver scarring occurs in all cases of ARPKD and is usually present at birth. Liver scarring can lead to decreased liver function and other liver problems. However, liver problems from ARPKD tend to become more of a concern over time.
High blood pressure. Most children with ARPKD have high blood pressure.8 High blood pressure increases a child’s chances of heart disease and stroke. High blood pressure can also further damage a child’s kidneys.
How do health care providers diagnose ARPKD?
Health care providers diagnose ARPKD with ultrasound imaging. The test can show enlarged kidneys and liver scarring.
How do health care providers treat the complications of ARPKD?
Enlarged kidney. Kidney enlargement cannot be prevented or reversed. One or both kidneys may need to be removed if their size makes breathing impossible. Children who don’t have working kidneys will need dialysis or a kidney transplant.
Growth failure. A health care provider may treat growth failure with nutritional therapy. In severe cases of growth failure, a health care provider and a child’s parents may consider treatment with human growth hormone. Human growth hormone is a prescribed, man-made hormone that can help children grow.
Breathing problems. Health care providers treat infants with breathing problems with artificial ventilation, which allows them to breathe with the help of a machine.
Kidney failure. Peritoneal dialysis is the preferred method of treating children with kidney failure, although health care providers also use hemodialysis. Kidney transplants may be a limited option for infants because of their size.
Liver problems. If serious liver disease develops, some children may need to have a combined liver and kidney transplant.
High blood pressure. A health care provider can help control blood pressure with medicines. Treating high blood pressure can help delay kidney failure.
References
Eating, Diet, & Nutrition for PKD
If you have any kind of chronic kidney disease, including polycystic kidney disease (PKD), talk with a dietitian about which foods to include in your diet and which foods might be harmful. Find a dietitian who specializes in helping people with kidney disease to help you choose the right foods and plan healthy meals.

PKD may require diet changes to help lower your blood pressure by limiting how much sodium (salt) you eat. Staying hydrated by drinking the right amount of fluid may help slow PKD’s progress toward kidney failure. Eating high-quality protein and smaller portions of protein also can help protect the kidneys. As your kidneys become more damaged, you may need to eat foods lower in phosphorus and potassium. Your health care provider will use lab tests to watch your levels of these minerals.
This content is provided as a service of the National Institute of Diabetes and Digestive and Kidney Diseases
(NIDDK), part of the National Institutes of Health. NIDDK translates and disseminates research findings to increase knowledge and understanding about health and disease among patients, health professionals, and the public. Content produced by NIDDK is carefully reviewed by NIDDK scientists and other experts.
