Kidney Failure
- What is Kidney Failure?
- Choosing a Treatment
- Hemodialysis
- Peritoneal Dialysis
- Kidney Transplant
- Conservative Management
- Eating Right
- Financial Help for Treatment of Kidney Failure
What is Kidney Failure?
In this section:
- What are the symptoms of kidney failure?
- What health problems can people with kidney disease develop?
- How can I live well with kidney failure?
- Can I be active with kidney failure?
- Will kidney failure affect my sleep?
- Will kidney failure affect my sex life?
- Can I keep working with kidney failure?
- How will kidney failure affect how I feel about my life?
- Who will be on my health care team?
If your kidney function drops below 15 percent of normal, you are said to have kidney failure. You may have symptoms from the buildup of waste products and extra water in your body.
To replace your lost kidney function, you may have one of three treatment options:
End-stage renal disease (ESRD) is kidney failure that is treated by dialysis or kidney transplant.
Some people with kidney failure choose not to have dialysis or a transplant but continue to receive care from their health care team, take medicines, and monitor their diet and lifestyle choices.
Work with your health care team and family to consider your options and choose a treatment that’s right for you. Treatment will help you feel better and live longer.
The more you know ahead of time about what to expect, the better prepared you may be to make a treatment choice and take charge of your care. You also need to give yourself time to get used to the big changes that will be happening in your life. Kidney failure will change your day-to-day activities and may change your relationships with friends and family, and how you feel.

What are the symptoms of kidney failure?
Symptoms of kidney failure may begin so slowly that you don’t notice them right away.
Healthy kidneys prevent the buildup of wastes and extra fluid in your body and balance the salts and minerals in your blood—such as calcium, phosphorus, sodium, and potassium. Your kidneys also make hormones that help control blood pressure, make red blood cells, and keep your bones strong.
Kidney failure means your kidneys no longer work well enough to do these jobs and, as a result, other health problems develop. As your kidney function goes down, you may
- have swelling, usually in your legs, feet, or ankles
- get headaches
- feel itchy
- feel tired during the day and have sleep problems at night
- feel sick to your stomach, lose your sense of taste, not feel hungry, or lose weight
- make little or no urine
- have muscle cramps, weakness, or numbness
- have pain, stiffness, or fluid in your joints
- feel confused, have trouble focusing, or have memory problems
Following your treatment plan can help you avoid or address most of these symptoms. Your treatment plan may include regular dialysis treatments or a kidney transplant, a special eating plan, physical activity, and medicines.
What health problems can people with kidney disease develop?
Kidney disease can lead to other health problems. Your health care team will work with you to help you avoid or manage:
High blood pressure. High blood pressure can be both a cause and a result of kidney disease. High blood pressure damages your kidneys, and damaged kidneys don’t work as well to help control your blood pressure. With kidney failure, your kidneys can’t get rid of extra water. Taking in too much water can cause swelling, raise your blood pressure, and make your heart work harder.
Blood pressure-lowering medicines, limiting sodium and fluids in your diet, staying physically active, managing stress, and quitting smoking can help you control your blood pressure.
Heart disease. Kidney disease and heart disease share two of the same main causes: diabetes and high blood pressure. People with kidney disease are at high risk for heart disease, and people with heart disease are at high risk for kidney disease.
The steps that you take to manage your kidney disease, blood pressure, cholesterol, and blood glucose (if you have diabetes) will also help you prevent heart attacks or strokes.
Anemia. When kidneys are damaged, they don’t make enough erythropoietin (EPO), a hormone that helps make red blood cells. Red blood cells carry oxygen from your lungs to other parts of your body. When you have anemia, some organs—such as your brain and heart—may get less oxygen than they need and may not function as well as they should. Anemia can make you feel weak and lack energy.
Your health care professional may prescribe iron supplements. In some cases, your professional may prescribe medicines to help your body make more red blood cells.
Mineral and Bone Disorder. Healthy kidneys balance the levels of calcium and phosphorus in your blood and make hormones that help keep your bones strong. As kidney function drops, your kidneys
- make less of the hormone that helps your body absorb calcium. Like one domino knocking over another, the low level of calcium in your blood triggers the release of parathyroid hormone (PTH). PTH moves calcium from your bones into your blood. Too much PTH can also make you feel itchy.
- don’t remove as much phosphorus. Extra phosphorus in your blood also pulls calcium from your bones.
Without treatment, bones may become thin and weak. You may feel bone or joint pain. Changes to your eating plan, medicines, supplements, and dialysis may help.

Malnutrition. As your kidney disease gets worse, it can be a challenge to keep yourself well fed. You may not feel hungry, food may taste different, or you may lose interest in food. Infections and other stresses on your body can make it hard for your body to use the food you do eat. Working closely with a dietitian to be sure you’re eating enough of the right foods can have long-term benefits for people with kidney disease.
Feeling itchy. Itching is common and happens for different reasons. You may feel itchy because you have dry skin. Using a moisturizer may help. Or, you may feel itchy because you have too much phosphorus in your blood. Eating less phosphorus may help stop the itching. Your health care provider may prescribe a medicine called a phosphate binder for you to take with meals. These medicines keep the phosphorus in your food from entering your bloodstream.
UV light from sunlight or a light box helps some people find relief.
How can I live well with kidney failure?
Doing well with kidney failure is a challenge. You will feel better if you
- stick to your treatment schedule
- review your medicines with your health care provider at every visit and take your medicines as prescribed
- work with a dietitian to develop an eating plan that includes foods you enjoy eating while also helping your health
- stay active—take a walk or do some other physical activity that you enjoy
- stay in touch with your friends and family
Treatment with dialysis or transplant will help you feel better and live longer. Your health care team will work with you to create a treatment plan to address any health problems you have. Your treatment will include steps you can take to maintain your quality of life and activity level.
Your eating plan plays an important role. When you have kidney failure, what you eat and drink may help you maintain a healthy balance of salts, minerals, and fluids in your body.
Can I be active with kidney failure?
Yes. Physical activity is an important part of staying healthy when you have kidney failure. Being active makes your muscles, bones, and heart stronger. Physical activity also makes your blood travel through your body faster so your body gets more oxygen. Your body needs oxygen to use the energy from food.
You may find that physical activity can also improve your mood and make you feel better.
Talk with your doctor before you start a new exercise routine. Start slowly, with easier activities such as walking at a normal pace or gardening. Work up to harder activities such as walking briskly. Aim to be active on as many days as possible.

Will kidney failure affect my sleep?
People who have kidney failure may have trouble sleeping. Sleep loss can affect your quality of life, energy level, and mood. Restless leg syndrome, sleep apnea, pain, or itching may make it hard for you to sleep.
You can take a number of steps to improve your sleep habits. For example, physical activity during the day and a warm bath before bed may help you sleep better at night. Avoid caffeine after lunchtime. Avoid alcoholic drinks before bed. Avoid smoking.
Talk with your health care provider if you often feel sleepy during the day or have trouble sleeping at night. Health care providers can treat sleep disorders such as sleep apnea or restless leg syndrome.
Will kidney failure affect my sex life?
Kidney failure will affect your emotions, nerves, hormones, and energy levels, all of which may change your sexual relationships. Taking good care of yourself by managing your kidney disease and controlling your blood pressure and blood glucose levels can help prevent some sexual problems, such as erectile dysfunction. Getting counseling may help with some emotional problems, such as anxiety and depression, which can get in the way of having satisfying sex.
You may feel shy asking questions about your sex life, but your health care team has heard the same questions from other people. Your provider is trained to help you address concerns about your sex life.
Can I keep working with kidney failure?
Many people with kidney failure continue to work. KidneyWorks is a program to help people with kidney disease keep working. The program focuses on Americans with CKD whose kidneys have not yet failed or who are living with a transplant. If you are on dialysis, the information in the KidneyWorks paper may also provide tips to help you keep your job.
The Americans with Disabilities Act means that an employer can’t legally fire you just because you’re on dialysis or have had a kidney transplant. The law requires an employer to make reasonable changes to the workplace for a person with a disability. For example, your employer may give you lighter physical jobs or schedule your work hours around your dialysis sessions. If you’re on peritoneal dialysis, you’ll need space and time to change the dialysis solution in the middle of the work day. Most employers can make these adjustments.
If your employer isn’t willing to meet your needs, your dialysis clinic’s renal social worker may be able to help find a way to satisfy both you and your employer.

How will kidney failure affect how I feel about my life?
Coping with kidney failure can be stressful. Some of the steps that you are taking to manage your kidney disease are also healthy ways to cope with stress. For example, physical activity and sleep help reduce stress. Learn more about healthy ways to cope with stress.
Depression is common among people with a chronic, or long-term, illness. Depression can make it harder to manage your kidney disease. Ask for help if you feel down. Your health care team can help you. Talking with a support group, clergy member, friend, or family member who’ll listen to your feelings may help.
Treatment for depression is available.
Who will be on my health care team?
You’ll have a whole team of trained health care providers to help you live well with kidney failure. The following people may be part of your health care team:
Nephrologist. A doctor who specializes in kidney health and oversees your treatment.
Dialysis nurse. A dialysis nurse will monitor your in-center dialysis and will see you monthly if you’re doing home or peritoneal dialysis. The nurse will make sure you’re taking your medicines correctly and help you find ways to lessen the side effects of dialysis. If you do home hemodialysis or peritoneal dialysis, your dialysis nurse will teach you how to set up your treatment, take care of the equipment, and watch for infections or other problems.
Transplant coordinator. A specially trained nurse who will be your point of contact, arrange your appointments, and teach you what to do before and after the transplant.
Renal dietitian. A renal dietitian is trained to help people with kidney failure. Your dietitian will help you make choices about what to eat and drink to help your treatment work better so you’ll feel better.
Social worker. Dialysis clinics and transplant centers have a social worker who works with people who have ESRD. Your renal social worker can help you find answers to problems such as
- keeping a job or changing jobs
- getting help paying for treatments
- finding services to help with transportation or chores around the house
- finding counseling services to deal with family problems
Family and friends. Allowing your friends and family to help and sharing news about your kidney disease can make a big difference in how you feel. Studies show that being connected to other people can help your health.
A strong support system of family and friends can make it easier to deal with health problems and life changes. Be sure to spend time with friends or keep in touch with them by phone or email. Stay involved in activities that interest you.

You. Taking charge of your own medical care can help you feel more in control of your life. Take all your medicines and keep all your appointments. Work with your health care team to learn about different kidney failure treatments, and let them know what kind of treatment you want. Ask questions when your health care provider tells you something you don’t understand. If you choose home hemodialysis or peritoneal dialysis, tell your dialysis nurse about any problems you have with equipment or supplies. If you have a transplant, talk with your transplant coordinator if your medicines cause side effects. You are your own best advocate.
Choosing a Treatment
In this section:
- How soon should I start learning about what type of treatment to have?
- What are my treatment options for kidney failure?
- What are the basics about hemodialysis?
- What are the basics about peritoneal dialysis?
- Does dialysis cure kidney failure?
- When do I have to start dialysis?
- What are the basics about kidney transplant?
- What are the basics about conservative management?
- Can I eat the same foods with any kidney failure treatment?
- How can I decide which treatment is right for me?
- Can I stop or change my treatment once I start?
- What are some ways to pay for kidney failure treatment?
- What is an advance directive, and why would I want to prepare one?
As your kidney disease gets worse, your health care provider may talk with you about preparing for kidney failure. Talking early with your provider about your treatment options—and making a choice before you need any one of these treatments—helps you take charge of your care. Treatment will help you feel better and live longer.
Understanding the treatment you choose and getting used to the idea that you need this treatment takes time. Each type of treatment has pros and cons. Your choice of treatment will have a big effect on your daily life. By learning about the differences among treatment options, you can choose the one that will be best for you. The more you know about the types of treatment, the better prepared you may be to make a choice.

How soon should I start learning about what type of treatment to have?
Start learning early about treatment options—before you need one. You’ll have time to
- learn about the different treatment options
- talk with other people who are living with dialysis, a transplant, or conservative management
- share your thoughts with your family and loved ones so they can learn about your treatment choices, too
- work with your health care team to create a kidney failure treatment plan
- prepare yourself mentally and physically for the changes ahead
Creating a treatment plan and sharing it with your family gives you more control.

What are my treatment options for kidney failure?
You can choose one of three treatment options to filter your blood and take over a small part of the work your damaged kidneys can no longer do. A fourth option offers care without replacing the work of the kidneys. None of these treatments will help your kidneys get better. However, they all can help you feel better.
- Hemodialysis uses a machine to move your blood through a filter outside your body, removing wastes.
- Peritoneal dialysis uses the lining of your belly to filter your blood inside your body, removing wastes.
- Kidney transplant is surgery to place a healthy kidney from a person who has just died, or from a living person, into your body to filter your blood.
- Conservative management treats kidney failure without dialysis or a transplant. You’ll work with your health care team to manage symptoms and preserve your kidney function and quality of life as long as possible.
Doing well with kidney failure is a challenge, and it works best if you
- stick to your treatment schedule.
- review your medicines with your health care provider at every visit. You are the only one who knows how your body is responding to each of your medicines. It’s really important that your provider knows which medicines you are taking.
- follow a special eating plan.
- are active most days of the week.
What are the basics about hemodialysis?
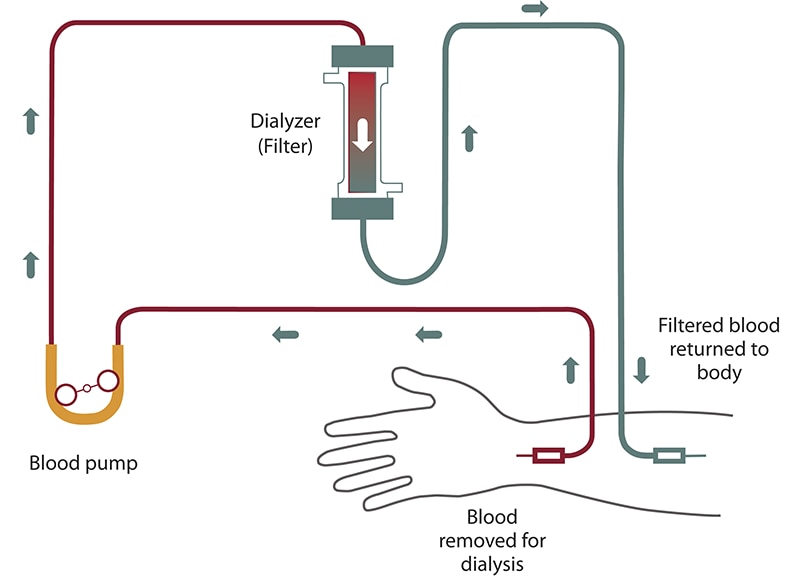
Hemodialysis can replace part of your kidney function. In hemodialysis, your blood goes through a filter outside your body and filtered blood is returned to your body. Hemodialysis
- filters your blood to remove harmful wastes and extra fluid
- helps control blood pressure
- helps balance important minerals, such as potassium, sodium, and calcium in your blood
Hemodialysis isn’t a cure for kidney failure, but it can help you feel better and live longer. You will also need to change what you eat, take medicines, and limit the amount of water and other liquids you drink and get from food.
Before you can start hemodialysis, you’ll need to have minor surgery to create a vascular access—a place on your body where you insert needles to allow your blood to flow from and return to your body during dialysis.
You can have hemodialysis at a dialysis center or in your home. Hemodialysis is usually done at a dialysis center three times a week, with each session lasting about 4 hours.
What are the pros and cons of in-center dialysis and home hemodialysis?
Pros: Dialysis center
- Dialysis centers are widely available in many parts of the country.
- Trained health care providers are with you at all times and help provide the treatment.
- You can get to know other people with kidney failure who also need hemodialysis.
- You don’t have to have a trained partner or keep equipment in your home.
Cons: Dialysis center
- The center arranges treatments, so your schedule is less flexible.
- You must travel to the center for treatment.
- A longer time between treatments means you will have the strictest limits on diet and liquids—because wastes and extra fluid can build up in your body. Having too much fluid in your blood can raise blood pressure and stress your heart. Removing too much fluid too fast during standard hemodialysis also can stress the heart.
- You may have more “ups and downs” in how you feel from day to day because of the longer time between treatments.
- Feeling better after a treatment may take a few hours.
Pros: Home hemodialysis
- You gain a sense of control over your treatments.
- You can choose what time to have the treatment; however, you should follow your doctor’s orders about how many times a week you need treatment.
- You don’t have to travel to a dialysis center.
- The flexible schedule makes it easier to work outside the home.
- You can travel with a hemodialysis machine or arrange for in-center treatment at your destination.
- You’ll have fewer “ups and downs” in how you feel from day to day because of more frequent treatments.
- You’ll have fewer limits on diet and liquids because the shorter time between sessions prevents waste and extra fluid buildup.
- You can spend more time with loved ones and doing other things because you don’t have to go to the dialysis center three times a week.
Cons: Home hemodialysis
- Not all dialysis centers offer home hemodialysis training and support.
- You and a family member or friend will have to set aside several weeks for training.
- Helping with treatments may be stressful for your treatment partner.
- You need space at home to store the hemodialysis machine and supplies.
- You’ll need to learn to put dialysis needles into your vascular access.
- Medicare and private insurance companies may limit the number of home hemodialysis treatments they will pay for. Few people can afford the costs for additional treatments.
What questions should I ask about hemodialysis?
You may want to ask your health care provider these questions:
- Is hemodialysis the best treatment choice for me? Why?
- If I’m treated at a dialysis center, can I go to the center of my choice?
- What should I look for in a dialysis center?
- Will my kidney doctor see me at the dialysis center?
- What does hemodialysis feel like?
- How will hemodialysis affect my ____ [blood pressure, diabetes, other conditions]?
- Is home hemodialysis available in my area? What type of training will I need? Who will train my partner and me?
- Will I be able to keep working? Can I have treatments at night? Will I be able to care for my children?
- How much should I exercise?
- Who do I contact if I have problems?
- Who will be on my health care team? How can the members of my health care team help me?
- If I do home hemodialysis, will my insurance pay for more than three sessions a week?
- Who can I talk with about finances, sex, or family concerns?
- Can I talk with someone who is on dialysis?
What are the basics about peritoneal dialysis?
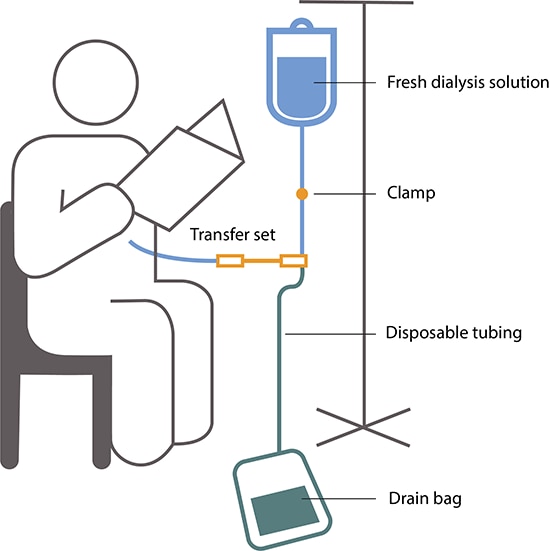
You do peritoneal dialysis at home. Peritoneal dialysis uses the lining of your belly to filter wastes and extra fluid from your body. This lining, called the peritoneum, surrounds your abdominal cavity and replaces part of your kidney function.
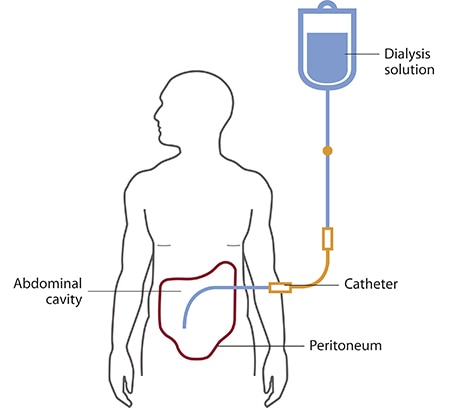
You’ll need to have minor surgery a few weeks before you start peritoneal dialysis. A doctor will place a soft tube, called a catheter, in your belly. The catheter stays in your belly permanently. When you start peritoneal dialysis, you’ll empty a kind of salty water, called dialysis solution, from a plastic bag through the catheter into your belly. When the bag is empty, you can disconnect your catheter from the bag so you can move around and do your normal activities. While the dialysis solution is inside your belly, it soaks up wastes and extra fluid from your body. After a few hours, you drain the used dialysis solution through another tube into a drain bag. You can throw away the used dialysis solution, now filled with wastes and extra fluid, in a toilet or tub. Then you start over with a fresh bag of dialysis solution. The process of emptying the used dialysis solution and refilling your belly with fresh solution is called an exchange.
You can choose which type of peritoneal dialysis will best fit your life.
- Continuous ambulatory peritoneal dialysis (CAPD)—An exchange takes about 30 to 40 minutes, and most people need to do four exchanges per day. You sleep with solution in your belly at night.
- Automated peritoneal dialysis, which uses a machine called a cycler to do three to five exchanges per night while you sleep. You may have to do one exchange during the day without the machine.
You may need a combination of CAPD and automated peritoneal dialysis if you weigh more than 175 pounds or if your peritoneum filters wastes slowly. For example, some people use a cycler at night and perform one exchange during the day. Others do four exchanges during the day and use a minicycler to perform one or more exchanges during the night. You’ll work with your health care team to find the best schedule for you.
What are the pros and cons of CAPD and automated peritoneal dialysis?
With either CAPD or automated peritoneal dialysis, you gain a sense of control over your treatments and don’t need the help of a partner. After you’re trained, you can do CAPD and automated peritoneal dialysis by yourself. With peritoneal dialysis, you’ll have boxes of dialysis solution taking up space in your home.
CAPD pros
- You don’t need a machine to do CAPD.
- You can do CAPD at the times you choose, as long as you complete the required number of exchanges each day.
- You can do CAPD in many locations.
- You can travel as long as you bring dialysis supplies with you or have them delivered to where you’re going.
CAPD cons
- CAPD can disrupt your daily routine.
- CAPD is a continuous treatment, and you need to do all exchanges 7 days a week.
Automated peritoneal dialysis pros
- You can do exchanges at night while you sleep.
- You may not have to perform exchanges during the day.
- You can travel as long as you bring dialysis supplies with you or have them delivered to where you’re going.
Automated peritoneal dialysis cons
- You need a machine. If you travel, you may have to carry your cycler with you.
- Your connection to the cycler limits your movement at night.
What questions should I ask about peritoneal dialysis?
You may want to ask your health care provider these questions:
- Is peritoneal dialysis the best treatment choice for me? Why? If yes, which type is best?
- What type of training do I need, and how long will it take?
- What does peritoneal dialysis feel like?
- How will peritoneal dialysis affect my ____ [blood pressure, diabetes, other conditions]?
- Will I be able to keep working?
- Will I be able to care for my children?
- How much should I exercise?
- Where do I store supplies?
- How often do I see my doctor?
- Who will be on my health care team? How can the members of my health care team help me?
- Who do I contact if I have problems?
- Who can I talk with about finances, sex, or family concerns?
- Can I talk with someone who is on peritoneal dialysis?
Learn about peritoneal dialysis.
Does dialysis cure kidney failure?
No. Even when very well done, dialysis only replaces part of your kidney function. Hemodialysis and peritoneal dialysis allow people with kidney failure to feel better and continue doing the things they enjoy, but neither replaces all of the jobs that healthy kidneys do. Over the years, kidney disease can cause other problems, such as heart disease, bone disease, arthritis, nerve damage, infertility, and malnutrition. These problems won’t go away with dialysis; however, doctors now have new and better ways to prevent or treat them. You should discuss these problems and their treatments with your doctor.
Watch a video of a doctor describing hemodialysis and peritoneal dialysis.
When do I have to start dialysis?
For most people, the need for dialysis comes on slowly. Symptoms, such as losing your desire to eat and losing muscle, may begin so slowly that you don’t notice them. Many people start dialysis when their kidney function (glomerular filtration rate) is between 5 and 10. When kidney function is this low, you may have symptoms from kidney failure and starting dialysis may help relieve them. Starting dialysis can help you regain your appetite and maintain your strength, which is harder to rebuild than it is to retain. Your health care provider can help you decide the best time to begin treatment.
What are the basics about kidney transplant?
Kidney transplant is surgery to place a healthy donor kidney into your body. A working, transplanted kidney does a better job filtering wastes and keeping you healthy than dialysis, but it still isn’t a cure.
When you have a transplant, surgeons usually leave your old kidneys in place and connect the donated kidney to an artery and a vein in your groin. The surgeon also transplants the ureter from the donor to let urine flow from your new kidney into your bladder. The transplanted kidney takes over the job of filtering your blood.
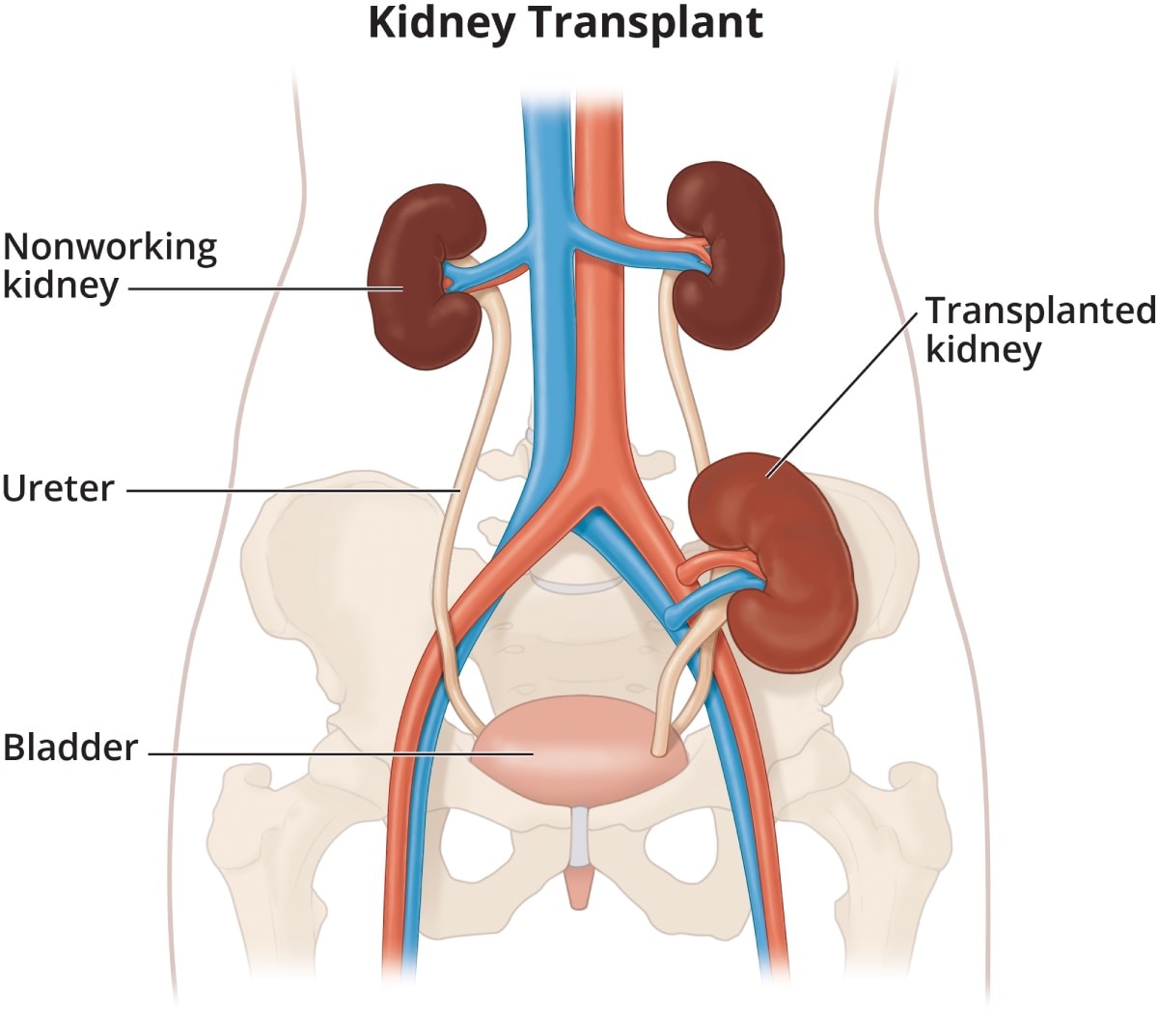
Your body normally attacks anything it sees as foreign, so to keep your body from attacking the donor kidney, you will need to take immunosuppressants —also called anti-rejection medicines. Like all strong medicines, anti-rejection medicines have side effects.
A transplant center can place you on the waiting list for a donor kidney if you have permanent kidney damage and your kidney function is 20 or less. While you’re waiting for a kidney transplant, you may need to start dialysis.
What are the pros and cons of a kidney transplant?
Together, you and your transplant team should weigh the pros and cons of a kidney transplant.
Pros
- A transplanted kidney works like a healthy kidney.
- If you have a living donor, you can choose the time of your operation.
- You may feel healthier and have a better quality of life.
- You’ll have fewer diet restrictions.
- You won’t need dialysis.
- People who get a donated kidney have a greater chance of living a longer life than those who stay on dialysis.
Cons
- A kidney transplant requires surgery, which involves certain risks, such as infection.
- You’ll go through extensive medical testing at the transplant clinic.
- You may need to wait years for a donor kidney.
- Your body may reject the donor kidney, so one transplant may not last a lifetime.
- You’ll need to take anti-rejection medicines—which may cause other health problems—for as long as the transplanted kidney works.
Watch a video about having a kidney transplant.
What questions should I ask about kidney transplant?
You may want to ask your doctor these questions:
- Is transplantation the best treatment choice for me? Why?
- What are my chances of having a successful transplant?
- How do I find out whether a family member or friend can donate?
- What are the risks to a family member or friend who donates?
- If a family member or friend does not donate, who will place me on a waiting list for a kidney?
- How long will I have to wait?
- How will I know if my donor kidney is working?
- How long does a transplanted kidney last?
- What are the side effects of anti-rejection medicines?
- Who will be on my transplant team? How can the members of my transplant team help me?
- Who can I talk with about finances, sex, or family concerns?
- Can I talk with someone who is living with a kidney transplant?
Learn about kidney transplant.
What are the basics about conservative management?
Conservative management for kidney failure means that your health care team continues your care without dialysis or a kidney transplant. The focus of care is on your quality of life and symptom control. The decision to start dialysis is yours. For most people, dialysis may extend and improve quality of life. For others who have serious conditions in addition to kidney failure, dialysis may seem like a burden that only prolongs suffering.
You have the right to decide how your kidney failure will be treated. You may want to speak with your family, doctor, counselor, or renal social worker—who helps people with kidney disease—to help you make this decision.
If you decide not to begin dialysis treatments, you may live for a few weeks or for several months, depending on your health and your remaining kidney function. Many of the complications of kidney failure can be treated with medicines, but only dialysis or transplant can filter wastes from your blood. As your kidney function declines, you may want to consider adding hospice, or end-of-life, care. You can have hospice care in a facility or at home. The hospice program is designed to meet end-of-life physical and emotional needs. Hospice care focuses on relieving pain and other symptoms.
Whether or not you choose to use hospice, your doctor can give you medicines to make you more comfortable. Your doctor can also give you medicines to treat the problems of kidney failure, such as anemia or weak bones. You may restart dialysis treatment if you change your mind.
What are the pros and cons of conservative management?
The pros and cons of conservative management depend on your current health status. Weigh the pros and cons with the help of your doctor.
What questions should I ask about conservative management?
If you’re thinking about conservative management, you may want to ask your doctor these questions:
- Is conservative management a treatment option for me to consider?
- Will dialysis improve my quality of life?
- Will dialysis prolong my life?
- Is there any downside to trying dialysis first?
- What should I do to prepare for conservative management?
- Who will continue to provide my care?
- Who will help my family?
- How long will I live?
- Will I be in pain?
- Can I stay at home?
- Where can I learn more about hospice?
- Who can I talk with about finances, advanced directives, sex, or family concerns?
Learn about conservative management.
Can I eat the same foods with any kidney failure treatment?
All of the treatment options for kidney failure require changes and limit what you may eat and drink.
Hemodialysis
Hemodialysis has the most restrictions. You will need to watch how much water and other liquids you get from food and drinks. You will also need to avoid getting too much sodium (a part of salt), potassium, and phosphorus. You may find it difficult to limit phosphorus because many foods that are high in phosphorus also provide the protein you need. Hemodialysis can remove protein from your body, so you will need to eat foods with high-quality protein such as meat, fish, and eggs. Avoiding foods such as beans, peas, nuts, tea, and colas will help you limit your phosphorus. You may also need to take a pill called a phosphate binder with your meals. Phosphate binders keep phosphorus in your food from entering your bloodstream. Talk with your dialysis center’s dietitian to find a hemodialysis meal plan that works for you.
Read about nutrition and eating right on hemodialysis.
Peritoneal dialysis
Like hemodialysis, peritoneal dialysis requires limits on sodium and phosphorus. You may need to take a phosphate binder. The liquid limitations in peritoneal dialysis may not be as strict as those for hemodialysis. In fact, you may need to drink more water and other liquids if your peritoneal dialysis treatments remove too much fluid from your body. Peritoneal dialysis removes potassium from the body, so you may need to eat potassium-rich foods such as potatoes, tomatoes, oranges, and bananas. However, you’ll have to be careful not to eat too much potassium because it can cause an unsteady heartbeat. Peritoneal dialysis removes even more protein than hemodialysis, so eating foods with high-quality protein will be important. You may need to limit calories because your body will absorb sugar from the dialysis solution.
Kidney transplantation
Kidney transplantation has the fewest restrictions on your diet. You will need to limit sodium because it can raise your blood pressure. Medicines that you take after the transplant can cause you to gain weight, so you may need to limit calories.
Conservative management
The diet for conservative management limits protein. Protein breaks down into waste products the kidneys must remove. Limiting protein may reduce the amount of work the kidneys have to do so they will last longer.
How can I decide which treatment is right for me?
Choosing the kidney failure treatment that is best for you may be hard. To make it easier
- start learning about your treatment options early
- think about how each treatment will affect your daily routine and how you feel
Talk with your doctor and with people who are on hemodialysis or peritoneal dialysis, or who’ve had a transplant, to find out the pros and cons of each treatment. Find out how the treatment changed their lives and the lives of those closest to them. Ask your doctor about the transplant waiting list, and about diet changes and medicines you’ll need with each treatment.
If you’re thinking about conservative management, ask your doctor how you’ll feel and how treatment can help keep you comfortable.
Reflect on what’s most important to you. If you plan to keep working, think about which treatment can make that easier. If spending time with family and friends means a lot to you, ask which treatment would give you the most free time. Find out which treatment would give you the best chance of feeling good and living longer.

You may wish to speak with your family, friends, health care team, spiritual advisor, or mental health counselor as you decide.
View a chart comparing hemodialysis, peritoneal dialysis, and kidney transplantation.
Can I stop or change my treatment once I start?
Yes. You can change your mind. If you don’t like your treatment choice, talk with your health care provider about trying something else.

What are some ways to pay for kidney failure treatment?
Medicare, the federal health insurance program, and private health insurance cover most of the cost. Medicare covers kidney failure no matter what your age. If you need more help to pay for treatment, state Medicaid programs provide funds for health care based on financial need. Your social worker can help you find more ways to pay for treatment.
What is an advance directive, and why would I want to prepare one?
You can make your treatment plans and wishes clear to health care providers and family members with an advance directive. During a medical crisis, you might not be able to tell your health care team and loved ones how you want to be treated or cared for. An advance directive is a written legal statement or document with your instructions either to provide or not provide certain treatments, such as dialysis, depending on what else is happening with your health. Advance directives may include
- a living will
- a durable power of attorney for health care decisions
- a do-not-resuscitate (DNR) order
Living will
A living will is a document that describes the conditions under which you would want to refuse treatment. You may state that you want your health care team to do everything possible to keep you alive, or you may request that they stop treatment, such as dialysis, if you fall into a coma from which you most likely won’t wake up.
In addition to dialysis, you may choose or refuse the following treatments to keep you alive:
- cardiopulmonary resuscitation (CPR)
- feedings through a tube in your stomach
- use of a machine to help you breathe
- medicines to treat infections
- surgery
- receiving blood
Refusing to have CPR is the same as a DNR order. If you choose to have a DNR order, your doctor will place the order in your medical chart.

Durable power of attorney for health care decisions
A durable power of attorney for health care decisions, or a health care proxy, is a document that names a person you choose to make health care decisions for you if you cannot make them for yourself. Make sure the person you name understands your values and will follow your instructions.
DNR order
A DNR order is a legal form that tells your health care team you do not want CPR or other life-sustaining treatment if your heart were to stop or if you were to stop breathing.
Each state has its own laws on advance directives. You can get a form for an advance medical directive that’s good in your state from the National Hospice and Palliative Care Organization.
Hemodialysis
In this section:
- What happens during hemodialysis?
- Where can I have hemodialysis?
- How do I prepare for hemodialysis?
- What changes will I have to make when I start hemodialysis?
- How will I know if my hemodialysis is working?
- What are possible problems from hemodialysis?
- What happens if I have been on dialysis and I decide to stop?
Hemodialysis is a treatment to filter wastes and water from your blood, as your kidneys did when they were healthy. Hemodialysis helps control blood pressure and balance important minerals, such as potassium, sodium, and calcium, in your blood.
Hemodialysis can help you feel better and live longer, but it’s not a cure for kidney failure.
What happens during hemodialysis?
During hemodialysis, your blood goes through a filter, called a dialyzer, outside your body. A dialyzer is sometimes called an “artificial kidney.”
At the start of a hemodialysis treatment, a dialysis nurse or technician places two needles into your arm. You may prefer to put in your own needles after you’re trained by your health care team. A numbing cream or spray can be used if placing the needles bothers you. Each needle is attached to a soft tube connected to the dialysis machine.
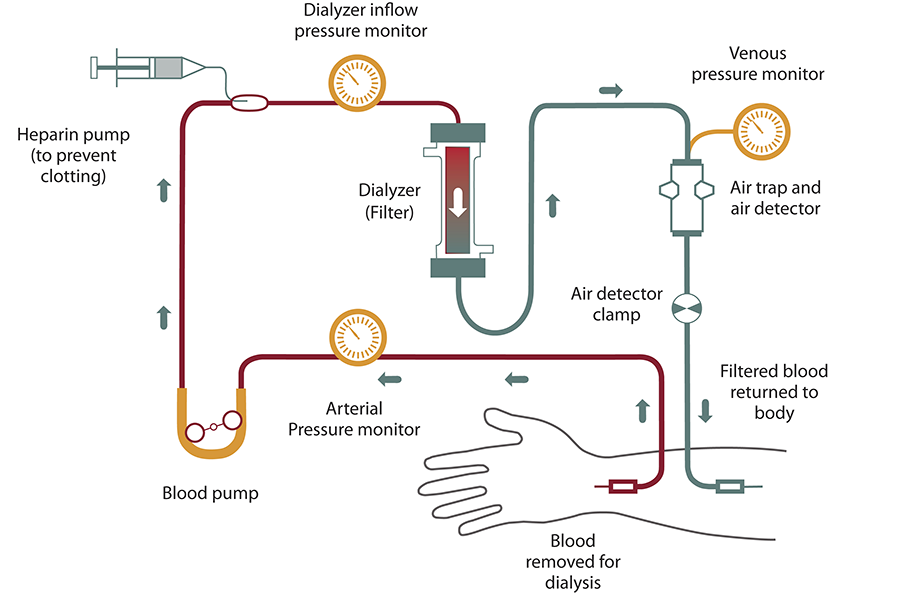
The dialysis machine pumps blood through the filter and returns the blood to your body. During the process, the dialysis machine checks your blood pressure and controls how quickly
- blood flows through the filter
- fluid is removed from your body
What happens to my blood while it’s in the filter?
Blood enters at one end of the filter and is forced into many, very thin, hollow fibers. As your blood passes through the hollow fibers, dialysis solution passes in the opposite direction on the outside of the fibers. Waste products from your blood move into the dialysis solution. Filtered blood remains in the hollow fibers and returns to your body.
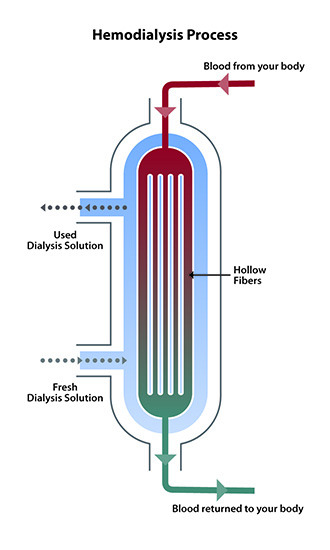
Your nephrologist—a doctor who specializes in kidney problems—will prescribe a dialysis solution to meet your needs. The dialysis solution contains water and chemicals that are added to safely remove wastes, extra salt, and fluid from your blood. Your doctor can adjust the balance of chemicals in the solution if
- your blood tests show your blood has too much or too little of certain minerals, such as potassium or calcium
- you have problems such as low blood pressure or muscle cramps during dialysis
Can the dialyzer do everything my kidneys once did?
No. Hemodialysis can replace part, but not all, of your kidney function. Dialysis will help improve your energy level, and changes you make to your diet can help you feel better. Limiting how much water and other liquid you drink and take in through foods can help keep too much fluid from building up in your body between treatments. Medicines also help you maintain your health while on dialysis.
Where can I have hemodialysis?
You can receive treatment at a dialysis center or at home. Each location has its pros and cons.
Dialysis center
Most people go to a dialysis center for treatment. At the dialysis center, health care professionals set up and help you connect to the dialysis machine. A team of health care workers will be available to help you. You will continue to see your doctor. Other team members may include nurses, health care technicians, a dietitian, and a social worker.
Set schedule
You’ll have a fixed time slot for your treatments, usually three times per week: Monday, Wednesday, and Friday; or Tuesday, Thursday, and Saturday. Each dialysis session lasts about 4 hours. When choosing a dialysis schedule, think about your work and child care or other caregiving duties.
Nighttime option
Some dialysis centers offer nighttime treatments. These treatments occur at the dialysis center 3 nights a week while you sleep, which takes longer. Getting longer overnight dialysis treatments means
- your days are free.
- you have fewer diet changes.
- your liquid allowance (how much liquid you can drink) is closer to normal.
- you may have a better quality of life than with a standard hemodialysis schedule. Longer treatment sessions may reduce your symptoms.
How do I find a dialysis center?
Your doctor, nurse, or social worker can help you find a dialysis center that’s convenient for you. Under Medicare rules, you have the right to choose the dialysis center where you’ll receive treatment. You may want to use Dialysis Facility Compare, which rates all dialysis centers according to quality. Your doctor will give your medical information to the dialysis center you choose.
Most large cities have more than one dialysis center to choose from. You can visit the centers to see which one best fits your needs. For example, you can ask about a center’s rules for laptop and cellphone use, as well as for having visitors. You may want the center to be close to your home to save travel time. If you live in a rural area, the closest dialysis center may be far from your home. If you’d have a hard time getting to the dialysis center, you may want to consider home dialysis treatments such as home hemodialysis or peritoneal dialysis.
Home hemodialysis
Home hemodialysis lets you have longer or more frequent dialysis, which comes closer to replacing the work healthy kidneys do—usually three to seven times per week, and with treatment sessions that last between 2 and 10 hours. Machines for home use are small enough to sit on an end table.
If you choose to have your treatments at home, you’ll still see your doctor once per month.
Flexible schedule
You can choose a schedule that fits the way you live. You can use
- standard home hemodialysis—three times a week or every other day for 3 to 5 hours
- short daily hemodialysis—5 to 7 days per week for 2 to 4 hours at a time
- nightly home hemodialysis—three to six times per week while you sleep
Your doctor will decide how many treatments you need each week for daily or nightly home hemodialysis.
More dialysis filters your blood more thoroughly
Compared with a standard hemodialysis schedule, daily or nightly home hemodialysis will let you
- eat and drink more normally
- take fewer blood pressure medicines
Healthy kidneys work 24 hours a day, 7 days a week. Getting more hemodialysis feels more like having healthy kidneys and lowers your chances for problems that are common with a standard hemodialysis schedule, such as
- painful muscle cramps from removing too much fluid too quickly
- high blood pressure, which can cause a headache or, in rare cases, a stroke
- low blood pressure, which can make you faint, feel sick to your stomach, or be more likely to fall
- high phosphate levels, which can weaken bones and make your skin itch
Better quality of life
Standard hemodialysis can make you feel tired or washed out for several hours after each treatment. People who have switched from standard hemodialysis to longer or more frequent hemodialysis report they feel better, with more energy, less nausea, and better sleep. They also may report a better quality of life.1
Training for home hemodialysis
Most dialysis centers require that you have a trained partner in your home during hemodialysis treatments, so you must ask a family member or friend to go through the training with you. The clinic’s home-training nurse will teach you important safety skills.
During training, you and your care partner will learn to
- set up the machine
- take steps to prevent infection
- place needles into the vascular access
- respond to any alarms from the machine
- check your weight, temperature, blood pressure, and pulse
- record treatment details for the clinic
- clean the machine
- throw out used supplies safely
- track used supplies and order new ones
Training may take 4½ to 6 hours, 5 days a week, for 3 to 8 weeks. If you already know how to place the needles into your access, training may take less time.

The home-training nurse will make sure that you and your partner feel confident and may visit your home to help with your first at-home treatment. In addition to providing training and a hemodialysis machine that stays in your home, the dialysis center also provides 24-hour support if you have a question or problem. Some programs also monitor treatments over the internet.
Dialysis center and home hemodialysis comparison
Use the following chart to help you choose between treatment in a dialysis center or at home.
| Dialysis Center and Home Hemodialysis Comparison Chart | ||
|---|---|---|
| Dialysis center | Home | |
| Schedule | Three treatments a week for about 4 hours. Monday, Wednesday, Friday; or Tuesday, Thursday, Saturday. | Flexible. Three to seven short or long treatments per week at times that work best for you. |
| Availability | Available in most communities; may require travel in some rural areas. | Becoming more widely available as smaller equipment is developed. |
| Machine/supplies | The clinic has the machine and supplies. | The machine and 2- to 4-weeks’ worth of supplies are in the home. You may need minor changes in your home to connect the machine to electricity and water. |
| Training | The clinic teaches about treatments, diet, liquids, medicines, lab tests, etc. | You and a partner must attend 3 to 8 weeks of home hemodialysis training. |
| Diet and liquids | Strict limits on liquids, phosphorus, sodium, and potassium intake. | Fewer limits on liquids or diet, based on the amount of hemodialysis and lab tests. |
| Level of freedom | Less freedom on treatment days. May feel washed out and tired for hours after each treatment. | More freedom because you set the treatment schedule to meet the total amount prescribed. Work and travel are much easier. |
| Amount of work | Center staff members do hemodialysis tasks. They can teach you to do some tasks. | You and your partner must set up, run, and clean the machine; check vital signs; track the treatments and send in forms; and order supplies. |
| Payment | Medicare and most other health plans cover three hemodialysis treatments a week. | Medicare covers three hemodialysis treatments a week and may cover more for medical reasons; other health plans may cover all hemodialysis treatments. |
How do I prepare for hemodialysis?
Dialysis is a complex treatment that takes time to understand. Because most people don’t feel sick until shortly before starting dialysis, you’ll likely still feel well when your doctor first talks to you about getting ready for dialysis. No one wants to start you on dialysis before you need it, but it takes time to prepare for dialysis.
Take care of the blood vessels in your arms
It’s important for you to protect the veins in your arm prior to starting dialysis. If you have kidney disease, remind health care providers to draw blood and insert IV lines only in veins below your wrist; for example, ask them to use a vein in the back of your hand. If an arm vein is damaged by an IV line or by repeated blood draws, that vein may not be able to be used for dialysis.
Vascular access surgery
One important step before starting hemodialysis treatment is having minor surgery to create a vascular access. Your vascular access will be your lifeline through which you’ll connect to the dialyzer. Dialysis moves blood through the filter at a high rate. Blood flow is very strong. The machine withdraws and returns almost a pint of blood to your body every minute. The access will be the place on your body where you insert needles to allow your blood to flow from and return to your body at a high rate during dialysis.
Three types of vascular access exist
- an arteriovenous (AV) fistula
- an AV graft
- a catheter
Work closely with your nephrologist and vascular surgeon—a surgeon who works with blood vessels—to make sure the access is in place in plenty of time. Healing may take several months. The goal is for your access to be ready for use when you are ready for dialysis.
Watch a video of a doctor explaining vascular access.
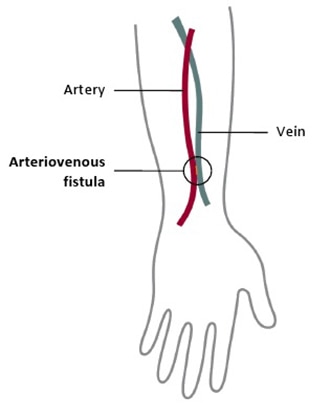
AV fistula
The best type of long-term access is an AV fistula. A surgeon connects an artery to a vein, usually in your arm, to create an AV fistula. An artery is a blood vessel that carries blood away from your heart. A vein is a blood vessel that carries blood back toward your heart. When the surgeon connects an artery to a vein, the vein grows wider and thicker, making it easier to place the needles for dialysis. The AV fistula also has a large diameter that allows your blood to flow out and back into your body quickly. The goal is to allow high blood flow so that the largest amount of blood can pass through the dialyzer.

The AV fistula is considered the best option because it
- provides highest blood flow for dialysis
- is less likely to become infected or clot
- lasts longer
Most people can go home after outpatient surgery. You will get local anesthesia to numb the area where the vascular surgeon creates the AV fistula. Depending on your situation, you may get general anesthesia and not be awake during the procedure.
Watch a video about why the fistula is the best access option.
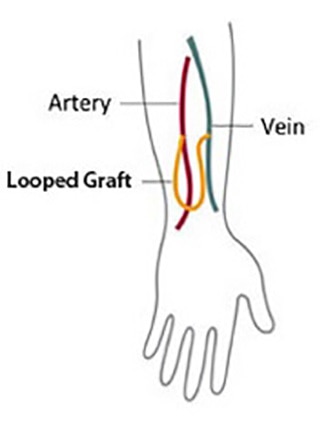
AV graft
If problems with your veins prevent you from having an AV fistula, you may need an AV graft instead. To create an AV graft, your surgeon uses a man-made tube to connect an artery to a vein. You can use an AV graft for dialysis soon after surgery. However, you’re more likely to have problems with infection and blood clots. Repeated blood clots can block the flow of blood through the graft and make it hard or impossible to have dialysis.
Catheter for temporary access
If your kidney disease has progressed quickly, or you have not had a vascular access placed before you need dialysis, you may need a venous catheter—a small, soft tube inserted into a vein in your neck, chest, or leg near the groin—as a temporary access. A nephrologist or an interventional radiologist—a doctor who uses medical imaging equipment to perform surgery—places the venous catheter while you’re in a hospital or at an outpatient clinic. You’ll receive local anesthesia and medicine to keep you calm and relaxed during the procedure.
Watch a video about problems with catheters.
What changes will I have to make when I start hemodialysis?
You have to adjust your life to build your dialysis treatment sessions into your routine. If you have in-center dialysis, you may need to rest after each treatment. Adjusting to the effects of kidney failure and the time you spend on dialysis can be hard. You may need to make changes in your work or home life, giving up some activities and responsibilities. Accepting these changes can be hard on you and your family. A mental health counselor or social worker can answer your questions and help you cope.
You will have to change what you eat and drink. Your health care team may adjust the medicines that you take.
Take care of your access
Your access is your lifeline. You will need to protect your access. Wash the area around your access with soap and warm water every day. Check the area for signs of infection, such as warmth or redness. When blood is flowing through your access and your access is working well, you can feel a vibration over the area. Let your dialysis center know if you can’t feel the vibration.
Make changes to what you eat and drink
If you’re on hemodialysis, you may need to limit
- sodium in foods and drinks.
- high-phosphorus foods.
- the amount of liquid you drink, including liquid found in foods. Fluid builds up in your body between hemodialysis treatments.
You may also need to
- add protein to your diet because hemodialysis removes protein
- choose foods with the right amount of potassium
- take vitamins made for people with kidney failure
- find healthy ways to add calories to your diet because you may not have a good appetite

Eating the right foods can help you feel better when you’re on hemodialysis. Talk with your dialysis center’s dietitian to find a hemodialysis meal plan that works for you.
How will I know if my hemodialysis is working?
You’ll know your hemodialysis treatments are working by how you feel. Your energy level may increase and you may have a better appetite. Hemodialysis reduces salt and fluid buildup, so you should have less shortness of breath and swelling as well.
This video explains how most people with kidney failure feel better after starting dialysis.
To make the most of your hemodialysis treatment, keep to your ideal “dry weight.” Your ideal dry weight is your weight when you don’t have extra fluid in your body. If you’re careful about the sodium in your diet and the hemodialysis is working, you should be able to reach your ideal dry weight at the end of every hemodialysis treatment. When hemodialysis treatments are working and you keep to your ideal dry weight, your blood pressure should be well controlled.

In addition, blood tests can show how well your hemodialysis treatments are working. Once a month, whether you’re on home or dialysis center hemodialysis, your dialysis center will test your blood. Read more about hemodialysis dose and adequacy.
What are possible problems from hemodialysis?
You could have a problem with your vascular access, which is the most common reason someone on hemodialysis needs to go to the hospital. Any type of vascular access may
- become infected
- have poor blood flow or blockage from a blood clot or scar
These problems can keep your treatments from working. You may need to have more procedures to replace or repair your access for it to work properly.
Sudden changes in your body’s water and chemical balance during treatment can cause additional problems, such as
- muscle cramps.
- a sudden drop in blood pressure, called hypotension. Hypotension can make you feel weak, dizzy, or sick to your stomach.
Your doctor can change your dialysis solution to help avoid these problems. The longer and more frequent treatments of home hemodialysis are less likely to cause muscle cramps or rapid changes in blood pressure than standard in-center dialysis.
You can lose blood if a needle comes out of your access or a tube comes out of the dialyzer. To prevent blood loss, dialysis machines have a blood leak detector that sets off an alarm. If this problem occurs at the clinic, a nurse or technician will be on hand to act. If you’re using home dialysis, your training will prepare you and your partner to fix the problem.
You may need a few months to adjust to hemodialysis. Always report problems to your health care team, who often can treat side effects quickly and easily. You can avoid many side effects by following an eating plan you develop with your dietitian, limiting liquid intake, and taking your medicines as directed.
What happens if I have been on dialysis and I decide to stop?
If you’ve been on dialysis and wish to stop, you’ll still receive supportive care. The dialysis social worker may be able to help you develop an end-of-life care plan before you stop dialysis.
References
Peritoneal Dialysis
You will find information about peritoneal dialysis on this page, including answers to the following questions:
- What is peritoneal dialysis and how does it work?
- What are the types of peritoneal dialysis?
- Where can I do peritoneal dialysis?
- How do I prepare for peritoneal dialysis?
- How do I perform an exchange?
- What changes will I have to make when I start peritoneal dialysis?
- What are the possible problems from peritoneal dialysis?
- How will I know if my peritoneal dialysis is working?
What is peritoneal dialysis and how does it work?
Peritoneal dialysis is a treatment for kidney failure that uses the lining of your abdomen, or belly, to filter your blood inside your body. Health care providers call this lining the peritoneum.
A few weeks before you start peritoneal dialysis, a surgeon places a soft tube, called a catheter, in your belly.
When you start treatment, dialysis solution—water with salt and other additives—flows from a bag through the catheter into your belly. When the bag is empty, you disconnect it and place a cap on your catheter so you can move around and do your normal activities. While the dialysis solution is inside your belly, it absorbs wastes and extra fluid from your body.
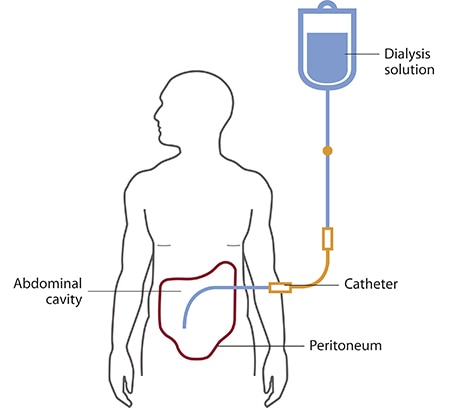
After a few hours, the solution and the wastes are drained out of your belly into the empty bag. You can throw away the used solution in a toilet or tub. Then, you start over with a fresh bag of dialysis solution. When the solution is fresh, it absorbs wastes quickly. As time passes, filtering slows. For this reason, you need to repeat the process of emptying the used solution and refilling your belly with fresh solution four to six times every day. This process is called an exchange.
You can do your exchanges during the day, or at night using a machine that pumps the fluid in and out. For the best results, it is important that you perform all of your exchanges as prescribed. Dialysis can help you feel better and live longer, but it is not a cure for kidney failure.
How will I feel when the dialysis solution is inside my belly?
You may feel the same as usual, or you may feel full or bloated. Your belly may enlarge a little. Some people need a larger size of clothing. You shouldn’t feel any pain. Most people look and feel normal despite a belly full of solution.
What are the types of peritoneal dialysis?
You can choose the type of peritoneal dialysis that best fits your life:
- continuous ambulatory peritoneal dialysis (CAPD)
- automated peritoneal dialysis
The main differences between the two types of peritoneal dialysis are
- the schedule of exchanges
- one uses a machine and the other is done by hand
If one type of peritoneal dialysis doesn’t suit you, talk with your doctor about trying the other type.
CAPD doesn’t use a machine. You do the exchanges during the day by hand.
You can do exchanges by hand in any clean, well-lit place. Each exchange takes about 30 to 40 minutes. During an exchange, you can read, talk, watch television, or sleep. With CAPD, you keep the solution in your belly for 4 to 6 hours or more. The time that the dialysis solution is in your belly is called the dwell time. Usually, you change the solution at least four times a day and sleep with solution in your belly at night. You do not have to wake up at night to do an exchange.
Automated peritoneal dialysis. A machine does the exchanges while you sleep.
With automated peritoneal dialysis, a machine called a cycler fills and empties your belly three to five times during the night. In the morning, you begin the day with fresh solution in your belly. You may leave this solution in your belly all day or do one exchange in the middle of the afternoon without the machine. People sometimes call this treatment continuous cycler-assisted peritoneal dialysis or CCPD.
Where can I do peritoneal dialysis?
You can do both CAPD and automated peritoneal dialysis in any clean, private place, including at home, at work, or when travelling.
Before you travel, you can have the manufacturer ship the supplies to where you’re going so they’ll be there when you get there. If you use automated peritoneal dialysis, you’ll have to carry your machine with you or plan to do exchanges by hand while you’re away from home.
How do I prepare for peritoneal dialysis?
Surgery to put in your catheter
Before your first treatment, you will have surgery to place a catheter into your belly. Planning your catheter placement at least 3 weeks before your first exchange can improve treatment success.
Although you can use the catheter for dialysis as soon as it’s in place, the catheter tends to work better when you have 10 to 20 days to heal before starting a full schedule of exchanges.
Your surgeon will make a small cut, often below and a little to the side of your belly button, and then guide the catheter through the slit into your peritoneal cavity. You’ll receive general or local anesthesia, and you may need to stay overnight in the hospital. However, most people can go home after the procedure.
You’ll learn to care for the skin around the catheter, called the exit site, as part of your dialysis training.
Dialysis training
After training, most people can perform both types of peritoneal dialysis on their own. You’ll work with a dialysis nurse for 1 to 2 weeks to learn how to do exchanges and avoid infections. Most people bring a family member or friend to training. With a trained friend or family member, you’ll be prepared in case you have a sick day and need help with exchanges.
If you choose automated peritoneal dialysis, you’ll learn how to
- prepare the cycler
- connect the bags of dialysis solution
- place the drain tube
If you choose automated peritoneal dialysis, you also need to learn how to do exchanges by hand in case of a power failure or if you need an exchange during the day in addition to nighttime automated peritoneal dialysis.

How do I perform an exchange?
You’ll need the following supplies:
- transfer set
- dialysis solution
- supplies to keep your exit site clean
If you choose automated peritoneal dialysis you’ll need a cycler.
Your health care team will provide everything you need to begin peritoneal dialysis and help you arrange to have supplies such as dialysis solution and surgical masks delivered to your home, usually once a month. Careful hand washing before and wearing a surgical mask over your nose and mouth while you connect your catheter to the transfer set can help prevent infection.
Use a transfer set to connect your catheter to the dialysis solution
A transfer set is tubing that you use to connect your catheter to the bag of dialysis solution. When you first get your catheter, the section of tube that sticks out from your skin will have a secure cap on the end to prevent infection. A connector under the cap will attach to any type of transfer set.
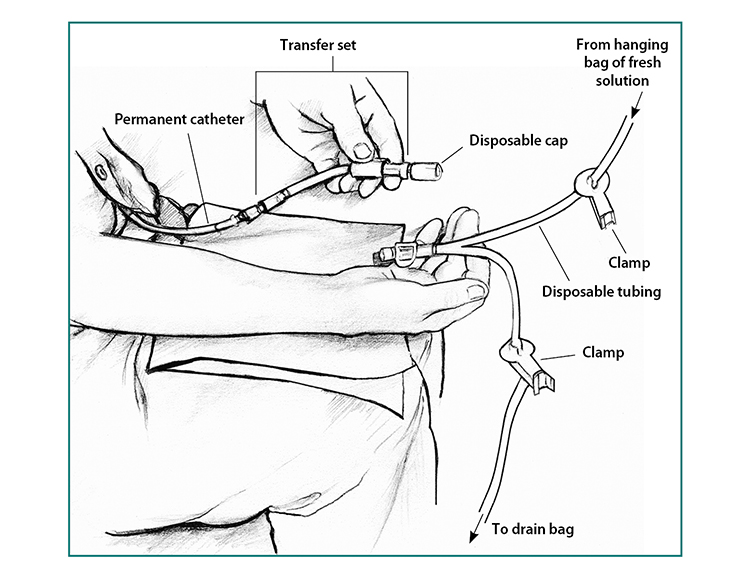
Between exchanges, you can keep your catheter and transfer set hidden inside your clothing. At the beginning of an exchange, you’ll remove the disposable cap from the transfer set and connect the set to a tube that branches like the letter Y. One branch of the Y-tube connects to the drain bag, while the other connects to the bag of fresh dialysis solution.
Use dialysis solution as prescribed
Dialysis solution comes in 1.5-, 2-, 2.5-, or 3-liter bags. Solutions contain a sugar called dextrose or a compound called icodextrin and minerals to pull the wastes and extra fluid from your blood into your belly. Different solutions have different strengths of dextrose or icodextrin. Your doctor will prescribe a formula that fits your needs.
You’ll need a clean space to store your bags of solution and other supplies.
Doing an exchange by hand
- After you wash your hands and put on your surgical mask, drain the used dialysis solution from your belly into the drain bag. Near the end of the drain, you may feel a mild tugging sensation that tells you most of the fluid is gone. Close the transfer set.
- Warm each bag of solution to body temperature before use. You can use an electric blanket, or let the bag sit in a tub of warm water. Most solution bags come in a protective outer wrapper, and you can warm them in a microwave. Don’t microwave a bag of solution after you have removed it from its wrapper.
- Hang the new bag of solution on a pole and connect it to the tubing.
- Remove air from the tubes—allow a small amount of fresh, warm solution to flow directly from the new bag of solution into the drain bag.
- Clamp the tube that goes to the drain bag.
- Open or reconnect the transfer set, and refill your belly with fresh dialysis solution from the hanging bag.
Using a cycler for automated peritoneal dialysis exchanges
In automated peritoneal dialysis, you use a machine called a cycler to fill and drain your belly. You can program the cycler to give you different amounts of dialysis solution at different times.
Each evening, you set up the machine to do three to five exchanges for you. You connect three to five bags of dialysis solution to tubing that goes into the cycler—one bag of solution for each exchange. The machine may have a special tube to connect the bag for the last exchange of the night.
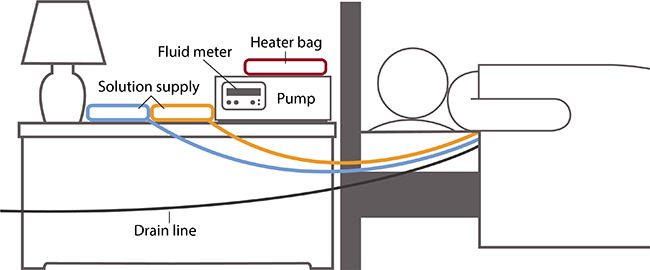
At the times you set, the cycler
- releases a clamp and allows used solution to drain out of your belly into the drain line
- warms the fresh dialysis solution before it enters your body
- releases a clamp to allow body-temperature solution to flow into your belly
A fluid meter in the cycler measures and records how much solution the cycler removes. Some cyclers compare the amount that was put in with the amount that drains out. This feature lets you and your doctor know if the treatment is removing enough fluid from your body.
Some cyclers allow you to use a long drain line that drains directly into your toilet or bathtub. Others have a disposal container.
What changes will I have to make when I start peritoneal dialysis?
Daily routine
Your schedule will change as you work your dialysis exchanges into your routine. If you do CAPD during the day, you have some control over when you do the exchanges. However, you’ll still need to stop your normal activities and take about 30 minutes to perform an exchange. If you do automated peritoneal dialysis, you’ll have to set up your cycler every night.
Physical activity
You may need to limit some physical activities when your belly is full of dialysis solution. You may still be active and play sports, but you should discuss your activities with your health care team.
Make changes to what you eat and drink
If you’re on peritoneal dialysis, you may need to limit
- sodium
- phosphorus
- calories in your eating plan
You may also need to
- watch how much liquid you drink and eat. Your dietitian will help you determine how much liquid you need to consume each day.
- add protein to your diet because peritoneal dialysis removes protein.
- choose foods with the right amount of potassium.
- take supplements made for people with kidney failure.
Eating the right foods can help you feel better while you’re on peritoneal dialysis. Talk with your dialysis center’s dietitian to find a meal plan that works for you.
Medicines
Your doctor may make changes to the medicines you take.
Coping
Adjusting to the effects of kidney failure and the time you spend on dialysis can be hard for both you and your family. You may
- have less energy
- need to give up some activities and duties at work or at home
A counselor or social worker can answer your questions and help you cope.
Take care of your exit site, supplies, and catheter to prevent infections
Your health care team will show you how to keep your catheter clean to prevent infections. Here are some general rules:
- Store your supplies in a cool, clean, dry place.
- Inspect each bag of solution for signs of contamination, such as cloudiness, before you use it.
- Find a clean, dry, well-lit space to perform your exchanges.
- Wash your hands every time you need to handle your catheter.
- Clean your skin where your catheter enters your body every day, as instructed by your health care team.
- Wear a surgical mask when performing exchanges.

What are the possible problems from peritoneal dialysis?
Possible problems from peritoneal dialysis include infection, hernia, and weight gain.
Infection
One of the most serious problems related to peritoneal dialysis is infection. You can get an infection of the skin around your catheter exit site or you can develop peritonitis, an infection in the fluid in your belly. Bacteria can enter your body through your catheter as you connect or disconnect it from the bags.
Seek immediate care if you have signs of infection
Signs of an exit site infection include redness, pus, swelling or bulging, and tenderness or pain at the exit site. Health care professionals treat infections at the exit site with antibiotics.
Peritonitis may cause
- pain in the abdomen
- fever
- nausea or vomiting
- redness or pain around your catheter
- unusual color or cloudiness in used dialysis solution
- the catheter cuff to push out from your body—the cuff is the part of the catheter that holds it in place
Health care professionals treat peritonitis with antibiotics. Antibiotics are added to the dialysis solution that you can usually take at home. Quick treatment may prevent additional problems.
Hernia
A hernia is an area of weakness in your abdominal muscle.
Peritoneal dialysis increases your risk for a hernia for a couple of reasons. First, you have an opening in your muscle for your catheter. Second, the weight of the dialysis solution within your belly puts pressure on your muscle. Hernias can occur near your belly button, near the exit site, or in your groin. If you have a swelling or new lump in your groin or belly, talk with your health care professional.
Weight gain from fluid and dextrose
The longer the dialysis solution remains in your belly, the more dextrose your body will absorb from the dialysis solution. This can cause weight gain over time.
Limit weight gain
With CAPD, you might have a problem with the long overnight dwell time. If your body absorbs too much fluid and dextrose overnight, you may be able to use a cycler to exchange your solution once while you sleep. This extra exchange will shorten your dwell time, keep your body from absorbing too much fluid and dextrose, and filter more wastes and extra fluid from your body.
With automated peritoneal dialysis, you may absorb too much solution during the daytime exchange, which has a long dwell time. You may need an extra exchange in the midafternoon to keep your body from absorbing too much solution and to remove more wastes and extra fluid from your body.
Your dietitian can provide helpful guidance to reduce weight gain.
How will I know if my peritoneal dialysis is working?
To find out if your dialysis exchanges are removing enough wastes, you’ll have a blood test and collect used dialysis solution once a month. If you’re still urinating, you may need to collect urine.
These tests help your doctor prescribe a dialysis schedule and dose to meet your health needs. If your dialysis schedule isn’t removing enough wastes or your body is absorbing too much dextrose, your doctor will make adjustments. Read about peritoneal dialysis dose and adequacy.
Kidney Transplant
In this section:
- What is the process for getting a kidney transplant?
- Who is on my transplant team?
- How will I feel after my transplant?
- How do I know my new kidney is working?
- What are the possible problems after a kidney transplant?
- What are the symptoms of transplant rejection?
- What are the side effects of anti-rejection medicines?
- What should I eat or avoid eating with a kidney transplant?
- How do I pay for my transplant?
Some people with kidney failure may be able to have a kidney transplant. During transplant surgery, a healthy kidney from a donor is placed into your body. The new, donated kidney does the work that your two kidneys used to do.
The donated kidney can come from someone you don’t know who has recently died (deceased donor), or from a living person—a relative, spouse, or friend. Due to the shortage of kidneys, patients on the waiting list for a deceased donor kidney may wait many years.
A kidney transplant is a treatment for kidney failure; it’s not a cure. You will need to take medicines every day to make sure your immune system doesn't reject the new kidney. You will also need to see your health care professional regularly.
A working transplanted kidney does a better job of filtering wastes and keeping you healthy than dialysis. However, a kidney transplant isn’t for everyone. Your doctor may tell you that you’re not healthy enough for transplant surgery.
Watch a video about kidney transplant.
What is the process for getting a kidney transplant?
If you want a kidney transplant, the process includes these steps:
- Tell your doctor or nurse you want to have a kidney transplant.
- Your doctor will refer you to a transplant center for tests to see if you’re healthy enough to receive a transplant. Living donors need to be tested to make sure they’re healthy enough to donate a kidney.
- If you don’t have a living donor, you’ll be placed on a waiting list to receive a kidney. You’ll have monthly blood tests while you wait for a kidney.
- You must go to the hospital to have your transplant as soon as you learn a kidney is available. If you have a living donor, you can schedule the transplant in advance.
Talk with your doctor
The first step is to talk with your doctor to find out whether you’re a candidate for a transplant. If you’re on dialysis, your dialysis team will also be part of the process. If you and your doctor think a kidney transplant is right for you, your doctor will refer you to a transplant center.
Get tested at a transplant center
At the transplant center, you’ll meet members of your transplant team. You’ll have tests to make sure you’re a good candidate for transplant.
Tests will include blood tests and tests to check your heart and other organs—to make sure you’re healthy enough for surgery. Some conditions or illnesses could make a transplant less likely to succeed, such as cancer that is not in remission, or current substance abuse.
You’ll also have tests to check your mental and emotional health. The transplant team must be sure you’re prepared to care for a transplanted kidney. You’ll need to be able to understand and follow a schedule for taking the medicines you need after surgery.
In a process called cross-matching, the transplant team tests the donor’s blood against your blood to help predict whether your body’s immune system will accept or reject the new kidney. A kidney from a relative is more likely to be a better tissue match than a kidney from someone who is not related to you.
If a family member or friend wants to donate a kidney and is a good match, that person will need a health exam to make sure he or she is healthy enough to be a donor. If you have a living donor, you don’t need to be on a waiting list for a kidney and can schedule the surgery when it’s best for you, your donor, and your surgeon.
Testing and evaluation at the transplant center may take several visits over weeks to months.
Get on the waiting list
If your tests show you can have a transplant, your transplant center will add your name to the waiting list. Wait times can range from a few months to years. Most transplant centers give preference to people who‘ve been on the waiting list the longest. Other factors, such as your age, where you live, and your blood type, may make your wait longer or shorter.
A transplant center can place you on the waiting list for a donor kidney if your kidney function is 20 or less—even if you aren’t on dialysis. While you wait for a kidney transplant, you may need to start dialysis.
Have monthly blood tests
While you wait for a kidney, you’ll need monthly blood tests. The center must have a recent sample of your blood to match with any kidney that becomes available.
Have your kidney transplant
During kidney transplant surgery, a surgeon places a healthy kidney into your body. You’ll receive general anesthesia before the surgery. The surgery usually takes 3 or 4 hours. Unless your damaged kidneys cause infections or high blood pressure or are cancerous, they can stay in your body. Surgeons usually transplant a kidney into the lower abdomen near the groin.
If you’re on a waiting list for a donor kidney, you must go to the hospital to have your transplant surgery as soon as you learn that a kidney is available.
If a family member or friend is donating the kidney, you’ll schedule the surgery in advance. A kidney from a living donor doesn’t have to be transported from one site to another, so it may be in better condition than a kidney from a deceased donor. Your surgical team will operate on you and your donor at the same time, usually in side-by-side rooms. One surgeon will remove the kidney from the donor, while another prepares you to receive the donated kidney.
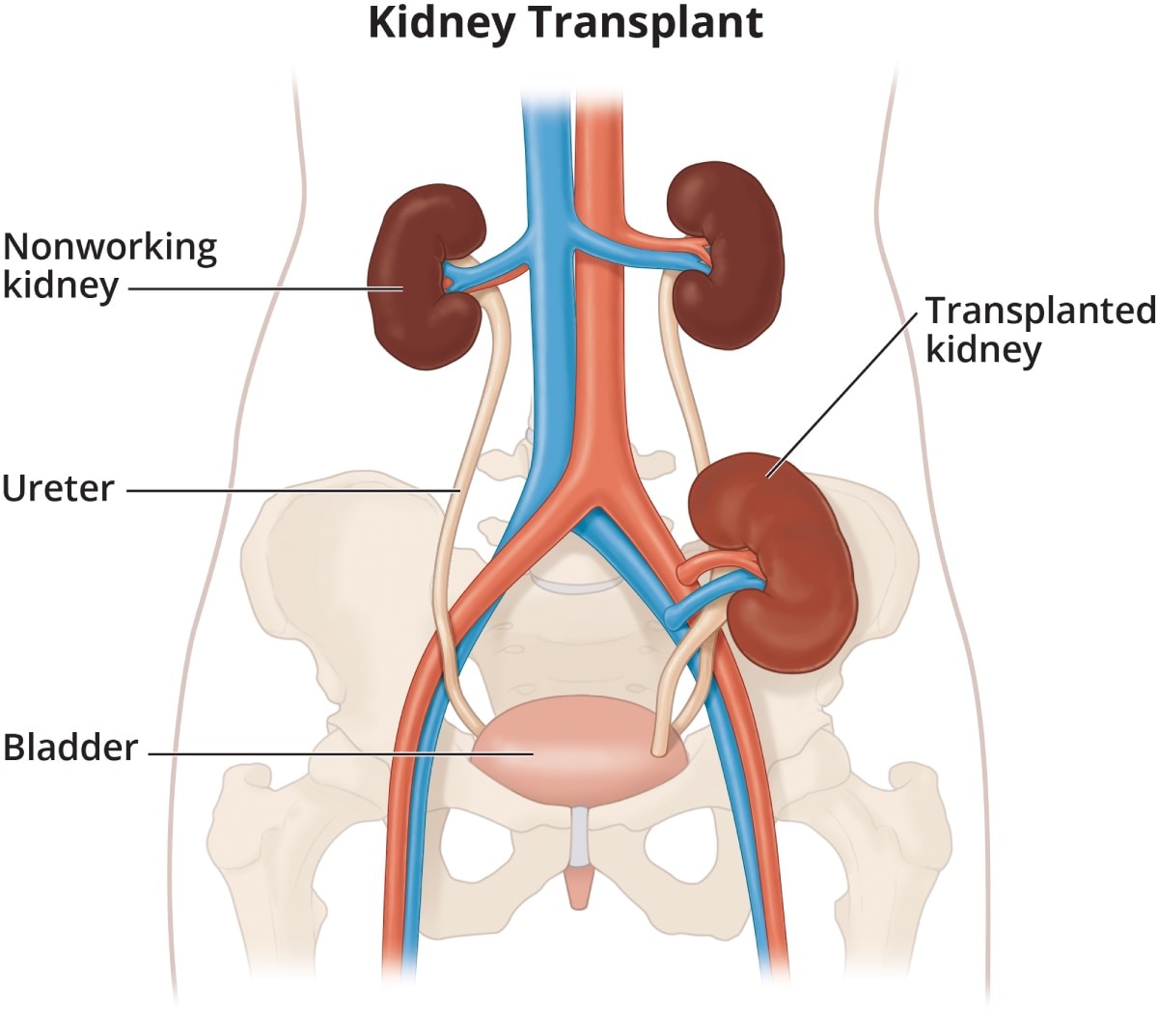
Who is on my transplant team?
A successful transplant involves working closely with your transplant team. Members of the team include:
- You—you are an important part of your transplant team.
- Your family members—this may include your spouse, parents, children or any other family member you would like to involve.
- Transplant surgeon—the doctor who places the kidney in your body.
- Nephrologist—a doctor who specializes in kidney health and may work closely with a nurse practitioner or a physician’s assistant.
- Transplant coordinator—a specially trained nurse who will be your point of contact, arrange your appointments, and teach you what to do before and after the transplant.
- Pharmacist—a person who tells you about all your medicines, fills your prescriptions, and helps you avoid unsafe medicine combinations and side effects.
- Social worker—a person trained to help you solve problems in your daily life and coordinate care needs after your transplant.
- Dietitian—an expert in food and nutrition who teaches you about the foods you should eat and avoid, and how to plan healthy meals.
Your transplant team will be able to provide the support and encouragement you need throughout the transplant process.

How will I feel after my transplant?
Many people report feeling much better right after having transplant surgery. For some people, it takes a few days for the new kidney to start working. You probably will need to stay in the hospital several days to recover from surgery—longer if you have any problems after the transplant. You’ll have regular follow-up visits with your nephrologist after leaving the hospital.
If you have a living donor, the donor will probably also stay in the hospital for several days. However, a new technique for removing a kidney for donation that uses a smaller cut may make it possible for the donor to leave the hospital in 2 to 3 days.
Before you leave the hospital, you need to learn how to stay healthy and take care of your donor kidney. You will have to take one or more anti-rejection medicines—also called immunosuppressants. Without medicine, your immune system may treat your donor kidney as foreign, or not your own, and attack your new kidney. Anti-rejection medicines may have side effects.
You may also need to take other medicines—for example, antibiotics to protect against infections. Your transplant team will teach you what each medicine is for and when to take each one. Be sure you understand the instructions for taking your medicines before you leave the hospital.

How do I know my new kidney is working?
Blood tests help you know your donor kidney is working. Before you leave the hospital, you’ll schedule an appointment at the transplant center to test your blood. The tests show how well your kidneys are removing wastes from your blood.
At first, you’ll need regular checkups and blood tests at the transplant center or from your doctor. As time goes on, you’ll have fewer checkups.
Your blood tests may show that your kidney is not removing wastes from your blood as well as it should. You also may have other symptoms that your body is rejecting your donor kidney. If you have these problems, your transplant surgeon or nephrologist may order a kidney biopsy.
What are the possible problems after a kidney transplant?
The donated kidney may start working right away or may take up to a few weeks to make urine. If the new kidney doesn’t start working right away, you’ll need dialysis treatments to filter wastes and extra salt and fluid from your body until it starts working.
Other problems following kidney transplant are similar to other pelvic surgeries and may include
- bleeding
- infection, especially a bladder infection
- hernia
- pain or numbness along the inner thigh that usually goes away without treatment
Transplant rejection is rare right after surgery and can take days or weeks to occur. Rejection is less common when the new kidney is from a living donor than when it’s from a deceased donor.
What are the symptoms of transplant rejection?
Transplant rejection often begins before you feel any changes. The routine blood tests that you have at the transplant center will reveal early signs of rejection. You may develop high blood pressure or notice swelling because your kidney isn’t getting rid of extra salt and fluid in your body.
Your health care provider will treat early signs of rejection by adjusting your medicines to help keep your body from rejecting your new kidney.
Transplant rejection is becoming less common. However, your body may still reject the donor kidney, even if you do everything you should. If that happens, you may need to go on dialysis and go back on the waiting list for another kidney. Some people are able to get a second kidney transplant.
Seek medical care right away
When you’re taking anti-rejection medicines, you’re at a greater risk for infection. Anti-rejection medicines can dull symptoms of problems such as infection. Call your transplant center right away if you aren’t feeling well or have
- a fever of more than 100 degrees
- drainage from your surgical scar
- burning when you pass urine
- a cold or cough that won’t go away
What are the side effects of anti-rejection medicines?
Some anti-rejection medicines may change your appearance. Your face may get fuller, you may gain weight, or you may develop acne or facial hair. Not all people have these side effects.
Anti-rejection medicines weaken your immune system, which can lead to infections. In some people over long periods of time, a weakened immune system can increase their risk of developing cancer. Some anti-rejection medicines cause cataracts, diabetes, extra stomach acid, high blood pressure, and bone disease.
When used over time, these medicines may also cause liver or kidney damage in some people. Your transplant team will order regular tests to monitor the levels of anti-rejection medicines in your blood and to measure your liver and kidney function.
What should I eat or avoid eating with a kidney transplant?
You have more choices about what to eat after you receive a kidney transplant than you would if you were on dialysis. However, you will need to work with a dietitian to develop an eating plan that can change in response to your medicines, test results, weight, and blood pressure.
Read more about kidney failure and eating, diet, and nutrition.
How do I pay for my transplant?
Medicare, the Federal Government health insurance program, will pay for transplant and care for 3 years after the transplant. Medicare will also pay for your donor’s surgery and his or her care. Watch a video about Medicare and kidney transplant.
Paying for medicines
Medicare and private insurance may help pay for your medicines. Additionally, drug companies give discounts to people who can show that they can’t afford to pay for their prescriptions. Talk with your transplant social worker to find out what resources may be available to help you pay for your transplant.
Read more about resources that may help pay for your kidney failure treatment.
Conservative Management
In this section:
- What is conservative management?
- What happens if I choose conservative management?
- Who chooses conservative management?
- What should I eat while on conservative management?
- How will I feel?
- How long can I live if I choose conservative management?
What is conservative management?
Conservative management for kidney failure means that your health care team continues your care without dialysis or a kidney transplant. The focus of care is on your quality of life and symptom control.
You have the right to decide how your kidney failure will be treated. You can choose conservative management instead of dialysis or transplant.

What are other names for conservative management?
You may hear conservative management called comprehensive conservative care, supportive care, nondialytic care, and comfort care. You also might hear the term “palliative care,” which is one part of conservative management. Palliative care addresses the physical, psychological, and spiritual needs of someone with a serious illness.
What happens if I choose conservative management?
Your health care team will help you create a plan to meet your care needs. Your health care team may include a nephrologist, primary care clinician, nurse, dietitian, social worker, and a pharmacist.
Treatment includes
- preserving kidney function for as long as possible
- managing your symptoms, such as nausea, poor appetite, and your feelings
- managing other health problems caused by kidney failure, such as anemia
- maintaining your quality of life for as long as possible
- preparing for end-of-life care
Conservative management won’t cure kidney disease. The treatment goals are to
- provide the best quality of life.
- avoid treatments and hospital stays that may worsen quality of life. This may mean fewer medical appointments, blood draws, and medicines.
Your care plan may change as your quality of life and health status change. As you near the end of your life, you may choose hospice care.

What is hospice?
Hospice (PDF, 132 KB) is a program of care and support for people at the end of life. A trained team of health professionals and caregivers provide symptom and pain relief as well as emotional and spiritual support. The hospice team also supports family caregivers.
With hospice care, you may choose to die at home or in a home-like hospice setting instead of in a hospital.
Medicare, the federal health insurance program, covers hospice care.
Who chooses conservative management?
People who wish to focus their care on the quality of their life may choose conservative management.
For most people, dialysis may extend and improve quality of life. For others, this is not true. Dialysis may not lengthen life for all people who have kidney failure and can feel like an added burden, especially for people who have other serious health problems. Dialysis may not prolong or improve the quality of life for people who
- are elderly and frail
- have other serious health problems, such as dementia, heart failure, or cancer
Your health care provider can help you and your family understand your health status so you can make an informed decision.
What should I eat while on conservative management?
What you eat and drink may make you feel better and may help prolong your life.1 Work with a dietitian to help you choose what to eat.

How will I feel?
As the waste products build up in your blood, your appetite may decline and you may become less alert. Your health care team can help you address these and other symptoms.
How long can I live if I choose conservative management?
The answer to this question is different for each person. If you need dialysis to survive and don’t receive it, you may live a few days or weeks.2

References
Eating Right
Why should I keep track of what I eat and drink?
The choices you make about what to eat and drink can help you feel better and can make your kidney failure treatments work better. Eating the right foods may give you more energy and strength.
Healthy kidneys balance the salts and minerals—such as calcium, phosphorus, sodium, and potassium—that circulate in your blood. When you have kidney failure, what you eat and drink may help you maintain a healthy balance of salts and minerals in your body.

The kind of kidney failure treatment you’ve chosen will affect your eating plan. If you have a kidney transplant, you’ll have fewer limits to your diet.
How can I learn what I should eat?
All dialysis and transplant centers have a dietitian who can help you plan your meals. A renal dietitian has special training in counseling people with kidney failure.
Nutrition counseling from a registered dietitian to help meet your medical or health goals is called medical nutrition therapy (MNT). Medicare pays for MNT for people with kidney disease with a written referral from your doctor. If you have insurance other than Medicare, ask if it covers MNT for kidney failure. You will also need a referral from your health care provider to a dietitian for MNT services.
You can find a registered dietitian online through the Academy of Nutrition and Dietetics or through your health care provider. Work closely with your dietitian to develop a meal plan that includes foods and drinks you enjoy eating while maintaining your health.
What will I need to change?
You will need to keep track of what you eat and drink. Changes may need to be made based on your blood test results. Nutrients are substances found in food that your body needs to function and maintain health—for example, water, sodium, protein, phosphorus, potassium, vitamins, and other minerals. Your diet can supply nutrients that are lost through treatment, or you might need to limit certain nutrients you eat that can build up in your body. You may also need to keep track of how many calories are in what you eat and drink.
You may need to keep track of the following:
Water
Water is in drinks such as coffee, tea, and soda; and in foods such as fruits, vegetables, ice cream, gelatin, soup, and popsicles. Your body needs water to function properly; however, in kidney failure, the kidneys can’t get rid of extra water. Taking in too much water can cause swelling, raise your blood pressure, and make your heart work harder.
Sodium
Sodium is a part of salt. You can find sodium in many canned, packaged, processed, and fast foods and in some seasonings. You need sodium to help control the amount of fluid in your body. However, too much sodium may cause high blood pressure. No matter what treatment you’re on, it’s likely you will need to limit sodium intake.

Protein
Protein provides the building blocks that help maintain and repair muscles, organs, and other parts of the body. Protein is in many foods you eat, including foods from animals and plants. Most diets include both types of protein. Too much protein can cause waste to build up in your blood, making your kidneys work harder.

Phosphorus
Phosphorus is balanced with calcium to keep your bones healthy. When you have kidney disease, phosphorus can build up in your blood. Too much phosphorus can weaken your bones.
Phosphorus is found naturally in foods rich in protein, such as meat, poultry, fish, nuts, beans, and dairy products. Phosphorus is also added to many processed foods, such as lunch meats. Phosphorus added to food may cause your blood levels to rise more than the phosphorus that is naturally found in food.
Your dietitian can help you find ways to get the protein you need without getting too much phosphorus.
Potassium
Potassium is a mineral that helps your nerves and muscles work. Potassium is found in fruits and vegetables such as oranges, bananas, tomatoes, and potatoes. Your nerve cells and brain will not work well if your potassium is too high or too low. If you have kidney failure, your potassium level may tend to be high. You may need to limit foods that are high in potassium.
Supplements for people with kidney failure
Supplements help provide some of the vitamins and minerals you may be missing, either because you need to avoid certain foods or because your treatment removes some vitamins from your body. Your health care professional may prescribe a supplement made for people with kidney failure. You should only take vitamin, mineral, or dietary supplements that your provider has recommended. Over-the-counter (no prescription needed) supplements not recommended by your providers may be harmful to you.
Calories
You need energy to fuel your body. Energy is measured in calories. Taking in more calories than your body uses can cause weight gain and high blood sugar. Taking in fewer calories than your body uses will result in weight loss.

Work with your dietitian to learn how you can make changes to what you eat and drink. Learn more about eating right for hemodialysis.
Financial Help for Treatment of Kidney Failure
In this section:
- Federal Government health insurance
- Joint federal-state programs
- Other federal programs
- Other state programs
- Private health insurance
- Help for special populations
- Help from private organizations
- Help paying for medicines
- Key Terms
Kidney failure treatment—hemodialysis, peritoneal dialysis, and kidney transplantation—is expensive. Many people with kidney failure need help paying for their care.
For many people with kidney failure, the Federal Government—through Medicare—helps pay for much of the cost of their treatment. The U.S. Congress passed the Social Security Amendments of 1972 that guarantee Medicare coverage for most people with kidney failure—even those under age 65.
You can also find financial help for kidney failure treatment from other sources, such as joint federal-state programs, private health insurance, private organizations, and medication assistance programs.
The amount you pay for premiums, copays, coinsurance, deductibles, prescriptions, and other costs is based on the services and medicines you need and the health care coverage you have. You can live for years with kidney failure, so it’s important that you get help to pay for your treatment.
Learn key terms about kidney failure costs, insurance, and financial aid.

Federal Government health insurance
What is Medicare?
Medicare is a federal health insurance program that pays health care costs for eligible people who are
- age 65 or older
- under age 65 with certain disabilities and those who have received Social Security Disability Insurance (SSDI) for 2 years
- of any age with end-stage renal disease (ESRD)—permanent kidney failure treated with a kidney transplant or blood-filtering treatments called dialysis
How can I get Medicare for kidney failure?
Visit Medicare.gov and search on “I have end-stage renal disease” to find information about whether you qualify for Medicare and how to sign up.
What health plans does Medicare offer?
Medicare has two main ways to get coverage—Original Medicare, which includes Part A and Part B, or a Medicare Advantage Plan, also called Part C. You can also choose to have prescription drug coverage through Medicare Part D.
Most people with kidney failure are not allowed to join a Medicare Advantage plan. However, beginning in 2021, the 21st Century Cures Act will allow people with ESRD to choose a Medicare Advantage plan instead of Original Medicare. Medicare Advantage plans may limit where you get care, but they cap out-of-pocket costs. With Original Medicare, there is no cap on out-of-pocket costs, but you can get care anywhere that Medicare is accepted.
You can find out more about the Medicare health plans by visiting Medicare.gov and searching on “ESRD,” then clicking on “Signing up for Medicare if you have ESRD.”
Other Medicare health plans are available that have special rules or are for specific groups of people. Medicare offers more information about these alternate plans online.
Learn more about Medicare benefits, rules, and coverage details at Medicare.gov or by calling 1-800-MEDICARE (1-800-633-4227; TTY: 1-877-486-2048).
When does Medicare coverage start for people with ESRD?
If kidney failure is the only reason you are signing up for Medicare, your Medicare start date will depend on the type of kidney failure treatment you receive. Find out more about when your Medicare coverage may start.
When does Medicare coverage end for people with ESRD?
If kidney failure is the only reason you have Medicare, your coverage end date will depend on whether you had a kidney transplant or dialysis treatment. Learn more about when your Medicare coverage will end.
Medicare coverage will not end if you are eligible because of age or disability.
How does Medicare coordinate with other coverage?
Learn more about which insurance pays first if you have Medicare and other health coverage.
Where can I get more information about Medicare’s kidney failure treatment coverage?
You can find more information about Medicare’s kidney failure treatment coverage from the following resources
- Medicare Coverage of Kidney Dialysis & Kidney Transplant Services
- Getting Started: Medicare’s Coverage of Dialysis & Kidney Transplant Benefits
- Getting Started: Medicare for Children with End-Stage Renal Disease (PDF, 3.55 MB)
Joint federal-state programs
You may also be able to get help paying for your kidney failure treatment from one or more programs that are run jointly by the Federal Government and state governments, including Medicaid and the Children’s Health Insurance Program (CHIP).
What is Medicaid?
Medicaid provides free or low-cost health coverage for some low-income people, families and children, pregnant women, the elderly, and people with disabilities. Each state runs its own Medicaid program based on rules set by the Federal Government. Medicaid may pay for services that Medicare does not.
Find out whether you qualify for Medicaid in your state and learn how to apply at
- Healthcare.gov, 1-800-318-2596 (TTY: 1-855-889-4325)
- National Association of Medicaid Directors state agency locator
Learn more at Medicaid.gov or call 1-877-267-2323 (TTY: 866-226-1819).
What is the Children’s Health Insurance Program (CHIP)?
CHIP offers free or low-cost Medicaid to children whose parents earn too much for Medicaid but not enough to pay for a private health plan. CHIP is run by the states, based on federal rules. In some states, CHIP may cover pregnant women and parents. Find out if your family members qualify for CHIP through Healthcare.gov or your state’s Medicaid or CHIP agency.
Learn more about CHIP at InsureKidsNow.gov, or call 1-877-543-7669.
Other federal programs
What other federal programs can help?
The Social Security Administration can provide financial help through two programs—Social Security Disability Insurance (SSDI) and Supplemental Security Income (SSI).
- SSDI pays a monthly amount to people who can’t work and have paid enough Social Security taxes. If you have an illness or injury that Social Security believes will keep you out of work for at least a year, SSDI payments may be an option. There is a 5-month waiting period before SSDI payments begin.
- SSI pays a monthly amount to disabled children and adults who earn little and don’t have many financial assets. A person who gets SSI may be able to get food stamps and Medicaid, too.
Read more about both SSDI and SSI and learn how to apply at SSA.gov or by calling 1-800-772-1213 (TTY: 1-800-325-0778).
Other state programs
What other state programs can help?
Medicare Savings Programs are programs in which your state may pay your Medicare premiums, deductibles, and/or coinsurance if you have a low income and few assets. How Medicaid works in U.S. territories varies. Learn more about how your state Medicaid works online.
State Health Insurance Assistance Programs (SHIPs) give local advice about health insurance to people who have Medicare or who are eligible for Medicare. SHIP counselors can help you choose the best plan for your needs. Find a SHIP counselor at shiptacenter.org or call 1-877-839-2675.
State kidney programs provide financial help and other services to people with kidney disease. Talk with your dialysis or transplant clinic social worker or financial counselor to find out if your state has a kidney program.
State Pharmaceutical Assistance Programs (SPAPs) help pay for prescription medicines in certain states. Learn what’s available in your state with the SPAP online locator.

Private health insurance
What types of private health insurance can help?
Some people with kidney failure use private health insurance to help pay for their health care
- Group health insurance. People buy this kind of health insurance through their employer, union, or a family member’s employer or union.
Group health plans pay for the first 30 months from the time you become eligible for Medicare for kidney failure. After that, a group plan can work with Medicare to help pay for costs that aren’t paid for by Medicare, such as copays, coinsurance, and deductibles. If you have or are eligible for group health insurance, you can contact the benefits administrator at the company or union that provides your insurance to find out what the plan covers and how it works with Medicare. - Individual health insurance. People buy this coverage for themselves and their families.
- The Health Insurance Marketplace offers health insurance plans to people who are legally present in the United States and who don’t have any other health insurance options. You can find, compare, and buy individual insurance plans in most states—or connect to your state’s insurance marketplace—at HealthCare.gov.
You cannot enroll in a Health Insurance Marketplace plan if you already have Medicare. Some people choose to keep their Marketplace plan instead of enrolling in Medicare. You may pay more for Medicare later if you don’t enroll in Medicare when you first become eligible. - Insurance companies, agents, brokers, and online insurance stores are other ways to find and buy individual health insurance plans. Learn how to find a trustworthy insurance company at USA.gov or by calling 1-844-USA-GOV1 (1-844-872-4681).
- The Health Insurance Marketplace offers health insurance plans to people who are legally present in the United States and who don’t have any other health insurance options. You can find, compare, and buy individual insurance plans in most states—or connect to your state’s insurance marketplace—at HealthCare.gov.
- Medigap, also called Medicare Supplemental Insurance. People buy this extra health insurance from a private company. Medigap plans help cover some costs that are not covered by Original Medicare, such as copays, coinsurance, and deductibles. If you’re 65, federal law protects your right to buy a Medigap plan. If you’re under 65 and are on dialysis, you may or may not be able to buy a Medigap policy from a licensed insurance company in your home state. Learn more online about Medigap rules, benefits, deadlines, and premiums.
Help for special populations
What help is available for special populations?
There are programs that help people who are members of specific populations
- U.S. veterans can get help with health costs from the U.S. Department of Veterans Affairs.
- Active-duty service members, military retirees, and their families may be able to get health care coverage through TRICARE.
- American Indians and Alaska Natives may be able to get help from the Indian Health Service.
- People with disabilities can find help from the U.S. Department of Labor, which offers resources such as information on benefits, civil rights, and employment.
- Job seekers with disabilities, including those with kidney failure, may find help with job training and support from the Social Security Administration’s Ticket to Work Program.
- People in need of a kidney transplant can get information on organ transplant from the United Network for Organ Sharing (UNOS), a government-sponsored organization that manages the nation’s organ transplant system.
- Potential organ donors who want to donate an organ—but cannot afford to—can apply for help to pay travel and living costs from the National Living Donor Assistance Program.
Help from private organizations
What private organizations can help?
Private organizations such as charities and foundations can help people with kidney disease and kidney failure. The National Kidney Foundation provides patient education, advocacy, and, in some cases, limited financial help, scholarships, or both (call 1-800-622-9010).
Help paying for medicines
Talk with your health care team if you have trouble paying for your medicines, including asking about cheaper options. Your team may suggest other ways to cut your costs, such as using mail-order pharmacies or contacting local aid programs.

Drug discount programs may help you find the medicines you need for free or at a lower cost. Try these resources
- BenefitsCheckUp. Seniors with limited incomes can search for help with medicines, health care, rent, and other needs through this service of the National Council on Aging.
- Blink Health. Blink Health has negotiated prices for 15,000 medicines that may cost less than you’d pay with your insurance online or at your local pharmacy.
- GoodRx. GoodRx compares prices and provides coupons for FDA-approved drugs at over 70,000 pharmacies. Your medicines may cost less with the coupon than with your insurance.
- Medicine Assistance Tool. Some drug manufacturers have programs that provide free or low-cost drugs to people who meet their guidelines.
- NeedyMeds. This organization lists programs that help pay for medicines and supplies. You can search by medicine or manufacturer name.
- RxAssist. An online resource that lists drug company assistance programs, state programs, discount drug cards, copay help, and more.
- Rx Outreach. A nonprofit, mail-order pharmacy that provides affordable medicine to people in need through its website or by phone at 1-888-RXO-1234 (1-888-796-1234).
- State Pharmaceutical Assistance Program. Some states have programs that limit drug costs for people with limited income or who are elderly.
Key Terms
Some terms listed here have many meanings; only those meanings that relate to the financial and medical aspects of kidney failure and its treatment are included.
coinsurance: an amount a person may still need to pay after a deductible for health care. The amount is most often a percentage, such as 20 percent.
coordination period: if a person has more than one health plan, a coordination period is used to figure out which plan pays first and for how long. For example, if a person has an employer group plan and Medicare, the employer group plan is the first payer for the first 30 months the person is eligible for Medicare.
copay (or copayment): an amount a person may have to pay for health care. A copay is often a set fee. A person might pay $10 or $20 for a health care provider visit or prescription.
deductible: an amount a person must pay for health care or prescriptions before the health plan(s) will pay.
network: a group of health care providers that gives members a discount. Some plans pay for health care and prescriptions only if received from a network provider.
out of network: health care providers who are not in a plan’s network. In some health plans, health care and prescriptions cost more if received from these providers.premium: an amount a person must pay periodically—monthly or quarterly—for Medicare, another health plan, or drug plan coverage.
social worker: a person who is trained to help people solve problems in their daily lives, especially people with disabilities or low incomes. A social worker may help with financial, employment, and emotional issues. Dialysis clinics and transplant centers must have a social worker with a Master of Social Work degree to help their patients.
This content is provided as a service of the National Institute of Diabetes and Digestive and Kidney Diseases
(NIDDK), part of the National Institutes of Health. NIDDK translates and disseminates research findings to increase knowledge and understanding about health and disease among patients, health professionals, and the public. Content produced by NIDDK is carefully reviewed by NIDDK scientists and other experts.
The NIDDK would like to thank:
Stephanie Mahooty, DNP, MSN, Renal Medicine Associates; Gayle Romancito, RN, Indian Health Service; Jane Schell, MD, Assistant Professor of Medicine, University of Pittsburgh, Section of Palliative Care and Medical Ethics, Division of Renal-Electrolyte
