Diabetes Overview
- What Is Diabetes?
- Symptoms & Causes
- Risk Factors for Type 2 Diabetes
- Preventing Type 2 Diabetes
- Diabetes Tests & Diagnosis
- Managing Diabetes
- Insulin, Medicines, & Other Diabetes Treatments
- Healthy Living with Diabetes
- Preventing Diabetes Problems
- Clinical Trials
What Is Diabetes?
Diabetes is a disease that occurs when your blood glucose, also called blood sugar, is too high. Glucose is your body’s main source of energy. Your body can make glucose, but glucose also comes from the food you eat.
Insulin is a hormone made by the pancreas that helps glucose get into your cells to be used for energy. If you have diabetes, your body doesn’t make enough—or any—insulin, or doesn’t use insulin properly. Glucose then stays in your blood and doesn’t reach your cells.
Diabetes raises the risk for damage to the eyes, kidneys, nerves, and heart. Diabetes is also linked to some types of cancer. Taking steps to prevent or manage diabetes may lower your risk of developing diabetes health problems.
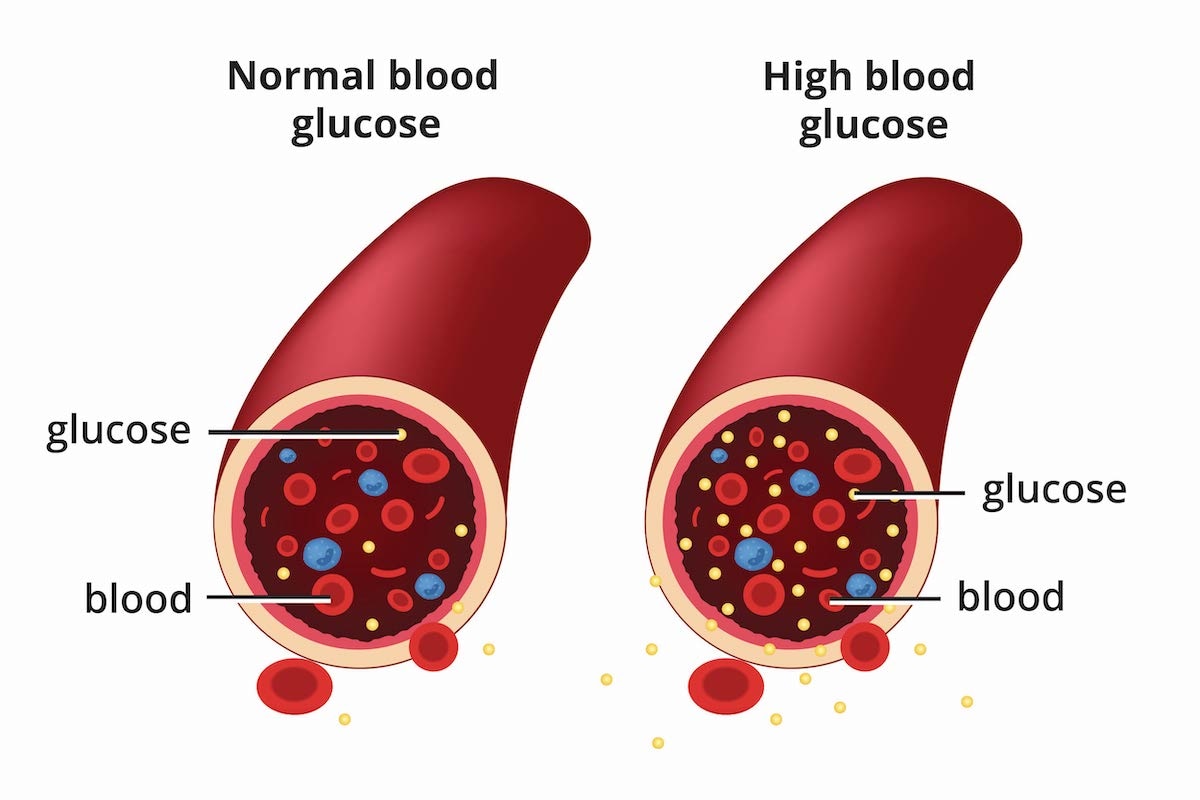 Diabetes is a disease that occurs when your blood glucose, also called blood sugar, is too high.
Diabetes is a disease that occurs when your blood glucose, also called blood sugar, is too high.
What are the different types of diabetes?
The most common types of diabetes are type 1, type 2, and gestational diabetes.
Type 1 diabetes
If you have type 1 diabetes, your body makes little or no insulin. Your immune system attacks and destroys the cells in your pancreas that make insulin. Type 1 diabetes is usually diagnosed in children and young adults, although it can appear at any age. People with type 1 diabetes need to take insulin every day to stay alive.
Type 2 diabetes
If you have type 2 diabetes, the cells in your body don’t use insulin properly. The pancreas may be making insulin but is not making enough insulin to keep your blood glucose level in the normal range. Type 2 diabetes is the most common type of diabetes. You are more likely to develop type 2 diabetes if you have risk factors, such as overweight or obesity, and a family history of the disease. You can develop type 2 diabetes at any age, even during childhood.
You can help delay or prevent type 2 diabetes by knowing the risk factors and taking steps toward a healthier lifestyle, such as losing weight or preventing weight gain.
Gestational diabetes
Gestational diabetes is a type of diabetes that develops during pregnancy. Most of the time, this type of diabetes goes away after the baby is born. However, if you’ve had gestational diabetes, you have a higher chance of developing type 2 diabetes later in life. Sometimes diabetes diagnosed during pregnancy is type 2 diabetes.
Prediabetes
People with prediabetes have blood glucose levels that are higher than normal but not high enough to be diagnosed with type 2 diabetes. If you have prediabetes, you have a higher risk of developing type 2 diabetes in the future. You also have a higher risk for heart disease than people with normal glucose levels.
Other types of diabetes
A less common type of diabetes, called monogenic diabetes, is caused by a change in a single gene. Diabetes can also come from having surgery to remove the pancreas, or from damage to the pancreas due to conditions such as cystic fibrosis or pancreatitis.
How common are diabetes and prediabetes?
More than 133 million Americans have diabetes or prediabetes.1
As of 2019, 37.3 million people—or 11.3% of the U.S. population—had diabetes.1 More than 1 in 4 people over the age of 65 had diabetes. Nearly 1 in 4 adults with diabetes didn’t know they had the disease.2
About 90% to 95% of diabetes cases are type 2 diabetes.3
In 2019, 96 million adults—38% of U.S. adults—had prediabetes.4
What other health problems can people with diabetes develop?
Over time, high blood glucose can damage your heart, kidneys, feet, and eyes. If you have diabetes, you can take steps to lower your chances of developing diabetes health problems by taking steps to improve your health and learning how to manage the disease. Managing your blood glucose, blood pressure, and cholesterol levels can help prevent future health problems.
 Managing your blood glucose levels can help prevent future health problems, such as damage to your eyes.
Managing your blood glucose levels can help prevent future health problems, such as damage to your eyes.
References
Symptoms & Causes
In this section:
- What are the symptoms of diabetes?
- What causes type 1 diabetes?
- What causes type 2 diabetes?
- What causes gestational diabetes?
- What else can cause diabetes?
- Clinical Trials for Symptoms and Causes of Diabetes
What are the symptoms of diabetes?
Common symptoms of diabetes include
- increased urination
- feeling very thirsty
- feeling very hungry, even after you have eaten
- blurred vision
- fatigue
- sores that do not heal
- frequent infections, such as urinary tract infections, skin infections, or yeast infections
There are different types of diabetes. People with any type of diabetes can have these symptoms. Some other symptoms, and how quickly the symptoms develop, depend on the type of diabetes that you have. Talk with your primary health care professional about any symptoms you are having and ask if you should be tested for diabetes. Your primary health care professional may be a doctor, physician assistant, or nurse practitioner.
Type 1 diabetes symptoms
In addition to some of the common diabetes symptoms listed above, people with type 1 diabetes may also have an unexplained weight loss. Most people don’t know they have type 1 diabetes until they develop diabetes symptoms.
Symptoms of type 1 diabetes usually develop quickly, over a few days or weeks. Type 1 diabetes is often diagnosed in children and young adults, but it can begin at any age. Children with type 1 diabetes typically develop symptoms over a short period of time. Common symptoms of type diabetes in children include
- having to urinate more often
- eating more but losing weight
- feeling very thirsty
These symptoms are less common in adults with type 1 diabetes. For some adults, symptoms of type 1 diabetes may develop slowly and seem more like type 2 diabetes. Some adults who develop diabetes may need special tests to find out what type of diabetes they have. Talk with your health care professional about the type of diabetes you may have. They can help you understand its causes and treatments.
Sometimes, people find out they have type 1 diabetes when they have signs and symptoms of a condition called diabetic ketoacidosis (DKA). Symptoms of DKA may include
- feeling very tired
- having trouble breathing
- having fruity-smelling breath
- fainting from dehydration
- having pain in your abdomen, nausea, or vomiting
If you have type 1 diabetes, your body doesn’t have enough insulin to use blood glucose—also called blood sugar—for energy. Your body will begin to use fat as a source of energy instead. This process produces substances called ketones. High levels of ketones can cause DKA, which is a medical emergency that needs to be treated right away.
DKA usually affects people with type 1 diabetes. People with type 2 diabetes may also develop DKA if their body doesn’t produce enough insulin.
Type 2 diabetes symptoms
Symptoms of type 2 diabetes can develop slowly, over several years. Many people with type 2 diabetes have no symptoms, or symptoms can be so mild that people might not even notice them. In addition to the common symptoms of diabetes listed above, people may find out they have type 2 diabetes when they develop symptoms of other health problems from diabetes. These include
- pain, numbness, or tingling in the feet or hands
- sexual problems
- chest pain
- vision loss
 Vision loss can be a symptom of diabetes.
Vision loss can be a symptom of diabetes.
Gestational diabetes symptoms
Gestational diabetes is a type of diabetes that may develop when you are pregnant. Most people with this type of diabetes have no symptoms. If you do have symptoms of gestational diabetes, they may be mild, such as being thirstier than usual or having to urinate more often.
People with a history of gestational diabetes are at higher risk of developing type 2 diabetes later in life. If you have a history of gestational diabetes, your health care professional may recommend regular testing for type 2 diabetes.
What causes type 1 diabetes?
Type 1 diabetes develops when the body’s immune system destroys the cells in the pancreas that make insulin. These cells are called beta cells. Genes and factors in the environment—the places where people live, play, work, study, and gather—may trigger the immune system to destroy beta cells in type 1 diabetes.
Insulin is a hormone that helps blood glucose get into the body’s cells to be used as energy. When your body doesn’t have enough insulin, glucose in your blood can’t get into the cells. As a result, your cells lack energy, your blood glucose level rises, and you develop diabetes.
Studies such as The Environmental Determinants of Diabetes in the Young (TEDDY) are trying to learn more about the causes of type 1 diabetes. Type 1 Diabetes TrialNet and other groups are working to find treatments that may prevent or slow the development of type 1 diabetes in people who are at risk for getting the disease.
What causes type 2 diabetes?
Type 2 diabetes is the most common form of diabetes. Type 2 diabetes develops when your pancreas doesn’t produce enough insulin, and your body has trouble using insulin, a condition called insulin resistance. Insulin resistance is when the cells in your muscles, fat, and liver don’t respond well to insulin. When there isn’t enough insulin to balance blood glucose levels, they begin to rise.
When blood glucose levels are higher than normal but not high enough to be diagnosed as type 2 diabetes, you have a condition called prediabetes. You have type 2 diabetes when health care professionals diagnose your blood glucose level as being too high.
Researchers don’t fully know what causes problems with insulin production and insulin resistance in type 2 diabetes. However, people are more likely to develop type 2 diabetes if they
- have overweight, obesity, or a large waist size.
- are age 35 or older. Children and teens can also develop type 2 diabetes, but the risk increases as a person gets older.
- have a family history of type 2 diabetes.
- are African American, American Indian, Asian American, Hispanic, Latino, or Pacific Islander.
- are not physically active, because of a job that requires sitting for long periods of time or because of difficulty moving their body.
- smoke, including tobacco products and e-cigarettes, or are exposed to secondhand smoke.
- have prediabetes.
- have a history of gestational diabetes, a type of diabetes that develops during pregnancy, or gave birth to a baby weighing 9 pounds or more.
You can’t change some of these risk factors, such as your age, family history, or race. However, you may be able to change some risk factors and prevent or delay type 2 diabetes by maintaining a healthy weight, being physically active, and stopping smoking.
 You may be able to prevent type 2 diabetes by maintaining a healthy weight and being physically active.
You may be able to prevent type 2 diabetes by maintaining a healthy weight and being physically active.
What causes gestational diabetes?
Gestational diabetes occurs when your body can’t make the extra insulin that you need during pregnancy. Scientists believe that substances made in your body, called hormones, may play a role in causing this form of diabetes.
Changes to hormones during pregnancy can make it harder for blood glucose to enter the cells in your body. This causes insulin resistance. In most pregnancies, the pancreas can make enough insulin to overcome these changes. If the pancreas can’t make enough insulin, you’ll develop gestational diabetes.
You’re more likely to develop gestational diabetes if you have certain risk factors, such as
- having overweight or obesity
- gaining too much weight during pregnancy
- having a family history of gestational diabetes, type 2 diabetes, or both
What else can cause diabetes?
Other causes of diabetes may include
- diseases caused by changes in your genes, also called gene variants
- endocrine diseases
- damage to or removal of the pancreas
- taking certain medicines
Diseases caused by changes in your genes
Gene variants are changes to certain genes. Some gene variants can cause diseases that can affect the pancreas and lead to diabetes.
Monogenic diabetes
Monogenic diabetes is a group of rare forms of diabetes caused by a variant, or change, in a single gene. Parents may pass these gene variants to their children. In some cases, a person may be the first one with the variant in the family. Most forms of monogenic diabetes reduce the amount of insulin your pancreas can make.
Cystic fibrosis
Cystic fibrosis is a genetic disease that leads to swelling and scarring in the pancreas. This scarring can prevent the pancreas from making enough insulin.
Hemochromatosis
Hemochromatosis is a genetic condition that causes your body and organs to build up harmful levels of iron. If the disease is not treated, high levels of iron may damage your pancreas and other organs.
Endocrine diseases
Some endocrine diseases make the body produce too much of certain hormones. High levels of these hormones may cause insulin resistance or diabetes. Endocrine diseases that may cause insulin resistance or diabetes include
- Cushing’s syndrome, which can cause the body to produce too much cortisol—often called the “stress hormone”
- acromegaly, which can cause the body to produce too much growth hormone
- hyperthyroidism, which can cause the body to produce too much thyroid hormone
- hypothyroidism, which can cause the body to produce too little thyroid hormone
Damage to or removal of the pancreas
The pancreas can be damaged by injury or diseases such as inflammation of the pancreas, also called pancreatitis. Diabetes may be the first sign of pancreatic cancer in older people without diabetes risk factors who develop diabetes. A damaged pancreas may make less insulin and lead to diabetes. In some cases, your pancreas may need to be removed. Without a pancreas, your body can’t produce insulin. You’ll develop diabetes and will have to take insulin.
Taking certain medicines
Certain medicines may harm the pancreas or affect the way insulin works in the body. Some of these medicines may include
- antipsychotics that are used to treat certain mental health problems
- antiseizure medicines that are used to treat epilepsy
- beta-blockers and diuretics that are used to treat high blood pressure
- glucocorticoids that are used to treat certain inflammatory diseases
- immunosuppressants that are used after an organ transplant
- niacin, a type of vitamin B that is sometimes used to treat high blood cholesterol
Statins, which are medicines to reduce LDL (“bad”) cholesterol levels, can slightly increase the chance that you’ll develop diabetes. However, statins help protect you from heart disease and stroke. For this reason, the strong benefits of taking statins outweigh the small chance that you could develop diabetes.
If you take medicines for these conditions, you may want to ask your primary health care professional if your medicines could affect your risk of developing diabetes.
Clinical Trials for Symptoms and Causes of Diabetes
NIDDK conducts and supports clinical trials in many diseases and conditions, including diabetes. The trials look to find new ways to prevent, detect, or treat diseases and improve quality of life.
What clinical trials study symptoms and causes of diabetes?
Clinical trials—and other types of clinical studies—are part of medical research and involve people like you. When you volunteer to take part in a clinical study, you help doctors and researchers learn more about disease and improve health care for people in the future.
Researchers are studying many aspects of symptoms and causes of diabetes, such as
- tests and treatments for rare and uncommon types of diabetes
- body changes in people who develop diabetes after having pancreatitis
Find out if clinical trials are right for you.
Watch a video of NIDDK Director Dr. Griffin P. Rodgers explaining the importance of participating in clinical trials.
What clinical trials about symptoms and causes of diabetes are looking for participants?
You can find clinical studies on symptoms and causes of diabetes at ClinicalTrials.gov. In addition to searching for federally funded studies, you can expand or narrow your search to include clinical studies from industry, universities, and individuals; however, the National Institutes of Health does not review these studies and cannot ensure they are safe for you. Always talk with your primary health care professional before you participate in a clinical study.
What have we learned about symptoms and causes of diabetes from NIDDK-funded research?
NIDDK has funded many research projects to learn more about symptoms and causes of diabetes.
- NIDDK-supported research helped scientists find genes linked to type 1 diabetes and new ways to identify people with type 1 diabetes before they develop symptoms.
- NIDDK also supported research to test medicines in people with type 1 diabetes before symptoms develop and before they require insulin-replacement therapy. In 2022, this research led to the U.S. Food and Drug Administration approval of a medicine (PDF, 101.1 KB) that may slow damage to the pancreas in early stages of type 1 diabetes.
- The Diabetes Prevention Program (DPP) studied how to prevent or delay disease in people at high risk of developing type 2 diabetes. The study found that participants who did regular physical activity and lost 5% to 7% of their body weight lowered their chance of developing type 2 diabetes.
- NIDDK funds the Glycemic Observation and Metabolic Outcomes in Mothers and Offspring (GO MOMS) study, which is investigating ways to improve gestational diabetes screening and diagnosis by better understanding blood glucose levels throughout pregnancy. GO MOMs will set the foundation for future ways to screen, diagnose, and treat high blood glucose levels during pregnancy.
- NIDDK supports the Rare and Atypical Diabetes Network (RADIANT) study, which is looking at ways to identify and define rare and atypical forms of diabetes.
- NIDDK formed the Type 1 Diabetes in Acute Pancreatitis Consortium (T1DAPC) to study type 1 diabetes and other types of diabetes that are related to acute pancreatitis. As part of this group, the Diabetes Related to Acute Pancreatitis and Its Mechanisms (DREAM) study is looking at people with recent acute pancreatitis to see how many develop diabetes.
Risk Factors for Type 2 Diabetes
Your chances of developing type 2 diabetes depend on a combination of risk factors. Although you can’t change risk factors related to family history, age, race, or ethnicity, you may be able to avoid some risk factors by maintaining a healthy weight and being physically active.1
Read about risk factors for type 2 diabetes below, and see which ones apply to you. Acting on the factors you can change may help delay or prevent type 2 diabetes.
What are the risk factors for type 2 diabetes?
 Diabetes type 2 can affect people at any age.
Diabetes type 2 can affect people at any age.
You can develop type 2 diabetes at any age, even during childhood. You are more likely to develop type 2 diabetes if you1
- are overweight or have obesity.
- are age 35 or older. Children and teens can also develop type 2 diabetes, but the risk increases as a person gets older.
- have a family history of diabetes.
- are African American, American Indian, Asian American, Hispanic/Latino, or Pacific Islander.
- are not physically active, because of physical limitations, a sedentary lifestyle, or a job that requires sitting for long periods of time.
- have prediabetes.
- have a history of gestational diabetes, a type of diabetes that develops during pregnancy, or gave birth to a baby weighing 9 pounds or more.
Children and teens are also at higher risk of developing type 2 diabetes if, in addition to the previous risk factors, they were born with a low birth weight or if their parent had gestational diabetes while pregnant with the child.1
You are encouraged to talk with a doctor about any of the health conditions listed above that may require medical treatment. Managing health problems may help reduce your chances of developing type 2 diabetes.2 Also, ask your doctor about any medicines you or your child take that might increase your risk. You can also take the Diabetes Risk Test to learn more about your risk for type 2 diabetes.
Does your weight put you at risk for type 2 diabetes?
If you have overweight or obesity, you may be able to prevent or delay type 2 diabetes by losing weight and being more physically active.1
To see if your weight may put you at risk for type 2 diabetes, learn your body mass index (BMI) and waist circumference.
Body mass index
Your BMI can help you tell if you are at a healthy weight or have overweight or obesity.
Most adults with a BMI of 25 or higher are overweight and have a higher risk of developing
type 2 diabetes.2 Asian Americans are overweight if their BMI is 23 or higher,1 while Pacific Islanders are overweight if their BMI is 26 or higher.3,4,5
If you are age 20 or older, use the BMI calculator for adults to learn your body mass index.
You can use a different BMI calculator for children or teens ages 2–19 years. This calculator uses BMI, sex, and age to estimate if a child or teen has overweight or obesity.
Waist circumference
Another way to estimate your risk of developing diabetes is to measure your waist circumference. Men have a higher risk of developing diabetes if their waist circumference is more than 40 inches, while women who are not pregnant have a higher risk if their waist circumference is more than 35 inches.6,7
Waist circumference is an indirect measurement of the amount of fat in your abdomen. Having a large waist circumference is a risk factor for diabetes and heart disease, even if you have a normal BMI.
References
Preventing Type 2 Diabetes
Perhaps you have learned that you have a high chance of developing type 2 diabetes, the most common type of diabetes. You might be overweight or have a parent, brother, or sister with type 2 diabetes. Maybe you had gestational diabetes, which is diabetes that develops during pregnancy. These are just a few examples of factors that can raise your chances of developing type 2 diabetes.
Diabetes can cause serious health problems, such as heart disease, stroke, and eye and foot problems. Prediabetes also can cause health problems. The good news is that type 2 diabetes can be delayed or even prevented. The longer you have diabetes, the more likely you are to develop health problems, so delaying diabetes by even a few years will benefit your health. You can help prevent or delay type 2 diabetes by losing a modest amount of weight by following a reduced-calorie eating plan and being physically active most days of the week. Ask your doctor if you should take the diabetes drug metformin to help prevent or delay type 2 diabetes.1
How can I lower my chances of developing type 2 diabetes?
Research such as the Diabetes Prevention Program shows that you can do a lot to reduce your chances of developing type 2 diabetes. Here are some things you can change to lower your risk:
- Lose weight and keep it off. You may be able to prevent or delay diabetes by losing 5 to 7 percent of your starting weight.1 For instance, if you weigh 200 pounds, your goal would be to lose about 10 to 14 pounds.
- Move more. Get at least 30 minutes of physical activity 5 days a week. If you have not been active, talk with your health care professional about which activities are best. Start slowly to build up to your goal.
- Eat healthy foods most of the time. Eat smaller portions to reduce the amount of calories you eat each day and help you lose weight. Choosing foods with less fat is another way to reduce calories. Drink water instead of sweetened beverages.
Ask your health care professional about what other changes you can make to prevent or delay type 2 diabetes.
Most often, your best chance for preventing type 2 diabetes is to make lifestyle changes that work for you long term. Get started with Your Game Plan to Prevent Type 2 Diabetes.

What should I do if my health care professional told me I have prediabetes?
Prediabetes is when your blood glucose, also called blood sugar, levels are higher than normal, but not high enough to be called diabetes. Having prediabetes is serious because it raises your chance of developing type 2 diabetes. Many of the same factors that raise your chance of developing type 2 diabetes put you at risk for prediabetes.
Other names for prediabetes include impaired fasting glucose or impaired glucose tolerance. Some people call prediabetes “borderline diabetes.”
About 1 in 3 Americans has prediabetes, according to recent diabetes statistics from the Centers for Disease Control and Prevention. You won’t know if you have prediabetes unless you are tested.
If you have prediabetes, you can lower your chance of developing type 2 diabetes. Lose weight if you need to, become more physically active, and follow a reduced-calorie eating plan.
Get started with Your Game Plan to Prevent Type 2 Diabetes. For more support, you can find a lifestyle change program near you through the National Diabetes Prevention Program.

If I had gestational diabetes when I was pregnant, how can I lower my chances of developing type 2 diabetes?
Gestational diabetes is a type of diabetes that develops during pregnancy. Most of the time, gestational diabetes goes away after your baby is born. Even if your gestational diabetes goes away, you still have a greater chance of developing type 2 diabetes within 5 to 10 years. Your child may also be more likely to become obese and develop type 2 diabetes later in life. Making healthy choices helps the whole family and may protect your child from becoming obese or developing diabetes.

Here are steps you should take for yourself and your child if you had gestational diabetes:
- Get tested for diabetes 6 to 12 weeks after your baby is born. If your blood glucose is still high, you may have type 2 diabetes. If your blood glucose is normal, you should get tested every 3 years to see if you have developed type 2 diabetes.
- Be more active and make healthy food choices to get back to a healthy weight.
- Breastfeed your baby. Breastfeeding gives your baby the right balance of nutrients and helps you burn calories.
- Ask your doctor if you should take the diabetes drug metformin to help prevent type 2 diabetes.1
References
Diabetes Tests & Diagnosis
In this section:
- Who should be tested for diabetes?
- What tests are used to diagnose diabetes?
- What test results tell me if I have diabetes or prediabetes?
- Which tests help my doctor know what kind of diabetes I have?
Your doctor can diagnose diabetes, prediabetes, and gestational diabetes using blood tests. The blood tests show if your blood glucose level, also called blood sugar, is higher than the range that is healthy for you. Blood tests can also help identify the type of diabetes you have.
Don’t try to diagnose yourself if you think you might have diabetes. Blood testing equipment that you can buy over the counter, such as a blood glucose meter, cannot diagnose diabetes.
Who should be tested for diabetes?
Anyone who has symptoms of diabetes should be tested for the disease. Some people will not have any symptoms but may have risk factors for type 2 diabetes and need to be tested. Most pregnant women should also be tested for gestational diabetes. Testing helps doctors find diabetes sooner, so they can work with their patients to manage the disease and prevent health problems.
If you have Medicare, it may cover the cost of tests if you have certain risk factors for diabetes. If you have different insurance, ask your insurance company if it covers diabetes tests.
 Blood tests help doctors diagnose diabetes and prediabetes.
Blood tests help doctors diagnose diabetes and prediabetes.
Type 1 diabetes
Doctors often diagnose type 1 diabetes in children and young adults when they have diabetes symptoms, such as feeling thirsty and having to urinate more often, or if they may have diabetic ketoacidosis. Symptoms in adults may be less specific.1
Type 1 diabetes can run in families. A study called TrialNet offers free testing to relatives of people with type 1 diabetes, even if the relatives don’t have symptoms.
Type 2 diabetes
Experts recommend routine testing for type 2 diabetes if you have certain risk factors. You may have a higher risk of developing type 2 diabetes if you are
- age 35 or older
- American Indian, Black or African American, Asian American, Hispanic/Latino, or Pacific Islander
- overweight or have obesity and have at least one other risk factor
- a woman who had gestational diabetes
Take the American Diabetes Association Diabetes Risk Test to see if you are at risk for type 2 diabetes.
Children can also develop type 2 diabetes. Experts recommend testing children and teens between the ages of 10 and 18 who are overweight or have obesity and have at least one more risk factor, such as a low birth weight, a parent who had diabetes while pregnant, or another factor.1
Adults and children with normal diabetes test results should be retested every 3 years.1
If your blood glucose levels are higher than the target range, but not high enough to be diagnosed with diabetes, doctors will diagnose you with prediabetes. Having prediabetes is serious because it raises the chance of developing type 2 diabetes. But developing type 2 diabetes can be prevented. Adults and children diagnosed with prediabetes should be tested for type 2 diabetes every year.
Testing for type 2 diabetes before and during pregnancy
All women who are planning to get pregnant should be tested for type 2 diabetes, especially if they have risk factors.
If you are already pregnant, you should be tested for type 2 diabetes at the first prenatal appointment, or in the first 15 weeks of pregnancy. If you have diabetes, you should receive special care during your pregnancy to avoid problems for you and the baby.
Gestational diabetes
All pregnant women who do not have a previous diagnosis of diabetes should be tested for gestational diabetes between 24 and 28 weeks of pregnancy.1
If you have gestational diabetes, you should get tested after your baby is born to see if you have type 2 diabetes, usually within 12 weeks after delivery.
What tests are used to diagnose diabetes?
Doctors use a variety of tests to diagnose diabetes and prediabetes. Your doctor may recommend different tests depending on whether you have symptoms or not, or whether you are pregnant.
Fasting plasma glucose test
The fasting plasma glucose (FPG) test measures your blood glucose level at a single point in time. For the most reliable results, your doctor will give you the test in the morning after you have fasted for at least 8 hours. Fasting means having nothing to eat or drink except sips of water.
A1C test
The A1C test is a blood test that provides your average levels of blood glucose over the last 3 months. Other names for the A1C test are hemoglobin A1C, HbA1C, glycated hemoglobin, and glycosylated hemoglobin test. You can eat and drink before this test. Before using the A1C test to diagnose diabetes, your doctor will consider factors, such as whether you are in your second or third trimester of pregnancy or whether you have certain types of anemia or another problem with your blood.1 The A1C test might not be accurate in those cases.
Certain types of hemoglobin, called hemoglobin variants, can interfere with measuring A1C levels. Most A1C tests used in the United States are not affected by the most common variants. If your A1C test results and blood glucose levels do not match, your doctor should consider that the A1C test may not be a reliable test for you.
Your doctor will report your A1C test result as a percentage, such as an A1C of 7%. The higher the percentage is, the higher your average blood glucose levels are.
Random plasma glucose test
Sometimes doctors use the random plasma glucose test to diagnose diabetes when you have symptoms of diabetes and they do not want to wait until you have fasted for 8 hours. You may have this blood test at any time.
Glucose challenge test
If you are pregnant, your doctor might test you for gestational diabetes with the glucose challenge test. Another name for this test is the glucose screening test. In this test, a health care professional will take a sample of your blood 1 hour after you drink a sweet liquid containing glucose. You do not need to fast for this test. If your blood glucose level is too high—135 mg/dL to 140 mg/dL or higher—you may need to return for an oral glucose tolerance test while fasting.
Oral glucose tolerance test
The oral glucose tolerance test (OGTT) helps doctors detect type 2 diabetes, prediabetes, and gestational diabetes. However, the OGTT is a more expensive test than the FPG test and the glucose challenge test, and it is not as easy to give.
Before the test, you will need to fast for at least 8 hours. A health care professional will take a blood sample to measure your glucose level after fasting. Next, you will drink a liquid that is high in sugar. Another blood sample is taken 2 hours later to check your blood glucose level. If your blood glucose level is high, you may have diabetes.
If you are pregnant, your blood will be drawn every hour for 2 to 3 hours. If your blood glucose levels are high two or more times during the OGTT, you may have gestational diabetes.
What test results tell me if I have diabetes or prediabetes?
Each test to detect diabetes and prediabetes uses a different measurement. Usually, your doctor will use a second test to confirm you have diabetes.
The table below helps you understand what your test results mean if you are not pregnant.1 If you are pregnant, some tests use different cutoffs. Ask your doctor what your test results mean.
Test results for diagnosis of prediabetes and diabetes
| Diagnosis | A1C | Fasting Plasma Glucose | Oral Glucose Tolerance Test* | Random Plasma Glucose Test‡ |
|---|---|---|---|---|
| Normal | below 5.7% | 99 mg/dL or below | 139 mg/dL or below | N/A |
| Prediabetes | 5.7% to 6.4% | 100 to 125 mg/dL | 140 to 199 mg/dL | N/A |
| Diabetes | 6.5% or above | 126 mg/dL or above | 200 mg/dL or above | 200 mg/dL or above |
Which tests help my doctor know what kind of diabetes I have?
Even though the tests described above can confirm you have diabetes, they can’t identify what type you have—type 1, type 2, or a rare type of diabetes called monogenic diabetes. Treatment can depend on the type of diabetes you have, so knowing which type you have is important.
Genetic testing
Genetic testing can diagnose most forms of monogenic diabetes, which is caused by a change—or mutation—in a gene. Anyone can have monogenic diabetes, but it is more common in babies who develop diabetes before they are 6 months old, some teens, and some young adults.
Autoantibodies
If you have diabetes, your doctor may look for certain autoantibodies to see if your diabetes is type 1. Autoantibodies are proteins in your immune system that mistakenly attack your healthy tissues and cells. A health care professional will take a sample of your blood for this test. If autoantibodies for diabetes are found in your blood, you may have type 1 diabetes.1
If you do not have diabetes but your parent or sibling has type 1 diabetes, your doctor might give you this test to see if you have a higher risk of developing type 1 diabetes. You may want to learn about diabetes symptoms and have follow-up testing as recommended by your doctor.1
Reference
Managing Diabetes
On this page:
- What are the diabetes ABCs?
- How can a healthy lifestyle help manage my diabetes?
- What types of medicines should I take?
- How can I check my blood glucose level at home?
- How can I keep track of my progress?
- What special situations should I plan for?
- Who should be on my health care team?
- Clinical Trials for Managing Diabetes
Diabetes can affect almost every part of your body, including your heart, eyes, kidneys, and nerves. Diabetes is also linked to some types of cancer. You may be able to prevent or delay diabetes health problems by leading a healthy lifestyle, taking your medicines, and managing your blood glucose level, also called blood sugar level. Work with your health care team to create a diabetes care plan that works for you.
What are the diabetes ABCs?
The diabetes ABCs can help you manage your blood glucose, blood pressure, and cholesterol levels. If you smoke, quitting is also important. Managing your ABCs may lower your chances of having health problems from diabetes, such as a heart attack, stroke, kidney disease, blindness, and foot or leg amputations.
A is for the A1C blood glucose test
The A1C test shows your average blood glucose level over the last 3 months. This test is done at a health care professional’s office or lab. For most people with diabetes, their goal is an A1C level below 7%.1 Your A1C goal may be different if you have other health problems.2 Ask your health care team how often you should have the test and what your goal should be.
B is for blood pressure
High blood pressure can damage your heart, kidneys, brain, and eyes. Some people with diabetes have a blood pressure goal below 130/80 mm Hg.2,3 If you have heart disease or are at high risk for diabetes health problems, your goal may be lower. Ask your health care team what your goal should be.
C is for cholesterol
Cholesterol is a fat, also called lipid, that is produced by your liver. Unhealthy levels of cholesterol in your blood can build up and clog your blood vessels, which may result in a heart attack or a stroke. Ask your health care team how often you need a cholesterol test, also called a lipid panel, and what your cholesterol level should be. Some people may need to take a medicine called a statin, or another medicine, to lower their cholesterol for heart health.
S is for stop smoking
Not smoking is important for your health, especially if you have diabetes. Both smoking and diabetes can make your blood vessels narrow. E-cigarettes aren’t a safe option either. If you smoke, vape, or use other tobacco products, stop. Ask for help so you don’t have to do it alone.
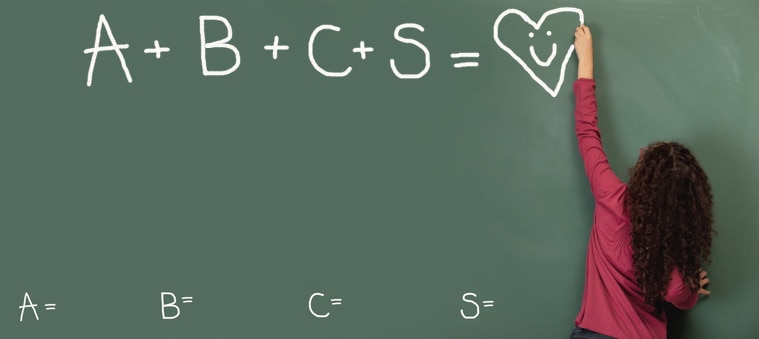 Follow your ABCs to keep your heart healthy. A is for the A1C blood glucose test, B is for blood pressure, C is for cholesterol, and S is for stop smoking.
Follow your ABCs to keep your heart healthy. A is for the A1C blood glucose test, B is for blood pressure, C is for cholesterol, and S is for stop smoking.How can a healthy lifestyle help manage my diabetes?
Staying healthy when you have diabetes can be a challenge. But leading a healthy lifestyle may help keep your blood glucose, blood pressure, and cholesterol levels in the ranges recommended by your health care team.
Create a healthy meal plan
You may worry that having diabetes means going without foods you enjoy. The good news is that you can still eat your favorite foods, but you might need to eat smaller portions or enjoy them less often. Work with your health care team, which may include a registered dietitian or a diabetes educator, to create a meal plan that works for you.
Talk with your health care team about any challenges you may have finding healthy food. A doctor, registered dietician, diabetes educator, or social worker may be able to recommend resources that can help you. The U.S. Department of Agriculture also provides a list of resources about affording healthy food and finding help from food assistance programs.
Get physical activity
Physical activity may help you lower blood glucose, blood pressure, and cholesterol levels. Being active may also help you get better sleep and improve your mood. Try to get at least 150 minutes of moderate-intensity physical activity, such as brisk walking, each week. If you can, try to do muscle-strengthening activities, such as wall push-ups or seated arm raises, two days a week.4
Reach and maintain a healthy weight
If you are overweight or have obesity, ask your health care team how you can manage your weight. To lose weight, you may need to consume fewer calories or get more physical activity. Your health care team may also recommend medicines or surgery to help manage your weight.
Get enough sleep
Getting enough sleep may improve your mood, energy level, and blood glucose level. Most adults should aim for about 7 to 8 hours each night.5 Children and adolescents may need more sleep.
Take care of your mental health
Feeling stressed, sad, or angry can be common for people with diabetes. Many people with chronic, or long-term, illnesses such as diabetes develop anxiety or other mental health conditions. Learn healthy ways to lower your stress, and ask for help from your health care team or a mental health professional.
 Being physically active can help you manage your diabetes.
Being physically active can help you manage your diabetes.What types of medicines should I take?
Taking diabetes medicines is often part of managing diabetes. The medicines you take depend on your type of diabetes, how well medicines control your blood glucose level, and other health conditions you may have. You may also need medicines to help manage blood pressure or cholesterol levels. Other factors such as medicine costs, insurance coverage, who is providing your diabetes care, and your lifestyle can also affect what medicines you take.
Take your medicines as they were prescribed, even if you feel good or have reached your blood glucose, blood pressure, or cholesterol goals. Avoid rationing your medicines or skipping taking your medicines if you have trouble paying for them. Talk with your health care team if you can’t afford your medicines or if you experience any side effects.
How can I check my blood glucose level at home?
If you take insulin or other diabetes medicines, checking your blood glucose level at home may help you avoid high or low blood glucose levels. Even if you do not use insulin, checking your blood glucose level at home can help you manage your diabetes. The test results may help you and your health care team make changes to your meal plan, physical activity level, or diabetes medicines. It may help you understand how certain types of food affect your blood glucose level. You do not get the same level of detail from blood tests—such as the A1C test—that you take at a health care professional’s office.
If you have type 1 diabetes, your health care team may ask you to check your urine at home for substances called ketones. A large amount of ketones in your urine may mean that you need to manage your diabetes more carefully. Work with your primary health care professional—who may be a doctor, physician assistant, or nurse practitioner—to change your diabetes care plan. If high levels of ketones are left untreated, you may develop a dangerous condition called diabetic ketoacidosis.
 Checking and recording your blood glucose level is an important part of managing diabetes.
Checking and recording your blood glucose level is an important part of managing diabetes.Devices to help manage diabetes
You can check your blood glucose level at home with a blood glucose meter. The meter tests a drop of your blood, usually from a prick of your fingertip. The meter will show you how much glucose is in your blood at that moment.
People who take insulin to manage their diabetes may benefit from using a continuous glucose monitor (CGM). A CGM uses a sensor in the tissue under your skin and shows changes in glucose levels throughout the day and night. Many CGM systems have alarms and warnings that let you know if your glucose level is too low or too high.
For safety, you may sometimes need to compare your CGM glucose readings with results from a standard blood glucose meter. This could be needed if you doubt the accuracy of your CGM readings, if you are changing your insulin dose, or if your CGM gives a warning alert.
Some people use a CGM as part of an artificial pancreas. An artificial pancreas is a system that mimics how a healthy pancreas controls blood glucose in the body. A CGM, an insulin pump, and a software program that shares information between the CGM and insulin pump make up the artificial pancreas.
Ask your health care team about the best way to check your blood glucose level and how often you should check it. Make sure to keep a record of your blood glucose self-checks, including the date and time you checked it, the results, and other information, such as what you ate or what physical activity you did that day. You can use a chart or a smartphone app to help you keep track. Take this information with you when you visit your health care team.
Recommended targets for blood glucose levels
Talk with your health care team about the blood glucose range that is healthy for you. Be sure to tell your health care team if your glucose levels frequently go above or below your target range.
Many people with diabetes aim to keep their blood glucose at these levels1
- Before a meal: 80 to 130 mg/dL
- About 2 hours after a meal starts: less than 180 mg/dL
Your blood glucose goals may be different if you are an adult over age 65 and have had diabetes for a long time. Your blood glucose goals may also be different if you have other health problems, like heart disease, or if your blood glucose often gets too low.
If you use a CGM, your health care team may ask you to keep track of your time in range. Time in range is the percentage of time that your glucose level stays in your target range. For many people with diabetes, the target range is between 70 and 180 mg/dL. Your health care team may adjust your diabetes care plan to help you stay in your target range at least 70% of the time.
Low blood glucose
When your blood glucose level is too low, it is called hypoglycemia. For most people with diabetes, the blood glucose level is too low when it is below 70 mg/dL.1,2 Talk with your primary care professional or health care team if you often have low blood glucose levels. Some people with low blood glucose experience symptoms such as
- feeling shaky or jittery
- headache
- cold sweat
If you often have low blood glucose levels, you may need to change your diabetes meal plan, physical activity plan, or medicines. Very low blood glucose may lead to confusion or fainting, and it can become a serious medical emergency that must be treated right away.
Glucagon—a hormone that raises blood glucose levels—is the best way to treat severely low blood glucose. Ask your health care team if you need a prescription for glucagon. If you have a glucagon prescription, you should teach your family, friends, and coworkers when and how to give you glucagon in case you are not able to do it yourself.
High blood glucose
When your blood glucose level is too high, it is called hyperglycemia. For most people with diabetes, the blood glucose level is too high when it is above 180 mg/dL. Talk with your health care team if you often have high blood glucose levels. Some people with high blood glucose have symptoms such as
- feeling tired
- feeling thirsty
- having blurry vision
- urinating too often
If you often have high blood glucose levels, you may need to make a change to your diabetes meal plan, physical activity plan, or medicines. Very high blood glucose may lead to confusion or fainting, and it may become a serious medical emergency that must be treated right away.
Checking urine for ketones
Your health care team may want you to check your urine for ketones if you have symptoms of diabetic ketoacidosis. Diabetic ketoacidosis is a medical emergency that needs to be treated right away.
Symptoms of diabetic ketoacidosis include
- feeling very tired
- having trouble breathing
- having fruity-smelling breath
- fainting
Most often, ketoacidosis affects people with type 1 diabetes. However, some people with type 2 diabetes can develop ketoacidosis if they do not produce enough insulin.
How can I keep track of my progress?
You may find it helpful to keep track of your ABCs and other important health information that you get during checkups with your primary care professional or other health care professionals. Download the Health Checkups Tracker (DOCX, 67.97 KB) , which includes information you may want to track. You can take this information with you when you visit your health care team. Talk with your primary care professional about your goals and whether you need to make any changes to your diabetes care plan.
What special situations should I plan for?
If you have diabetes, it is important to take care of your health no matter what is going on in your life. Ask your health care team if you should adjust your meal plan, activity level, or medicines in special situations, such as when you are sick, fasting, at school, planning to travel, or experiencing an emergency or natural disaster.
Who should be on my health care team?
You are the most important member of your health care team, but working with your health care team may help you improve your self-care. Most people with diabetes get help from a primary care professional, such as an internal medicine doctor, family doctor, pediatrician, physician assistant, or certified nurse practitioner trained in diabetes care. Ask your primary care professional about adding other members to your team, including
- a diabetes educator, nurse, or registered dietitian who can tell you more about your disease and how to improve your self-care
- a dentist to check for gum diseases and other dental problems
- an eye doctor to check for diabetic eye disease
- a pharmacist to help you with your medicines
- other specialists if you develop health problems such as heart disease, kidney disease, erectile dysfunction, or foot problems
- a social worker who may be able to help you find financial help for diabetes care and community resources
Write a list of questions before your visit with a health care professional so you don’t forget what you want to ask.
 When you see your health care professional, discuss your diabetes self-care plan, review your blood glucose chart or app, and ask questions.
When you see your health care professional, discuss your diabetes self-care plan, review your blood glucose chart or app, and ask questions.Clinical Trials for Managing Diabetes
NIDDK conducts and supports clinical trials in many diseases and conditions, including diabetes. The trials look to find new ways to prevent, detect, or treat diseases and improve quality of life.
What are clinical trials for managing diabetes?
Clinical trials—and other types of clinical studies—are part of medical research and involve people like you. When you volunteer to take part in a clinical study, you help health care professionals and researchers learn more about diseases and improve health care for people in the future.
Researchers are studying many aspects of managing diabetes, such as
- what are the best medicines to add to a diabetes care plan if a person with type 2 diabetes isn’t meeting their blood glucose targets using their current diabetes medicines
- how to train adolescents to support or care for family members with diabetes
- how treating obesity with weight-loss medicines or weight-loss surgery, also called metabolic and bariatric surgery, may help manage type 2 diabetes
- what different devices can help people with diabetes check their blood glucose level and inject insulin
Find out if clinical trials are right for you.
Watch a video of NIDDK Director Dr. Griffin P. Rodgers explaining the importance of participating in clinical trials.
What clinical trials for managing diabetes are looking for participants?
You can view a filtered list of clinical studies on managing diabetes that are federally funded, open, and recruiting at ClinicalTrials.gov. You can expand or narrow the list to include clinical studies from industry, universities, and individuals; however, the National Institutes of Health does not review these studies and cannot ensure they are safe for you. Always talk with your primary health care professional before you participate in a clinical study.
What have we learned about managing diabetes from NIDDK-funded research?
The research funded by NIDDK has improved quality of life for people with diabetes by finding better ways to diagnose and treat the disease.
Artificial pancreas
For decades, NIDDK has supported research that helped create artificial pancreas technology used by some people who need insulin to manage their diabetes.
NIDDK supported research that helped scientists develop the first continuous glucose monitor (CGM) that was approved by the U.S. Food and Drug Administration (FDA) in 1999. CGMs, which are part of artificial pancreas systems, help people track glucose levels in real-time with fewer finger pricks. Another major milestone came in 2016, when the FDA approved a commercial “hybrid” artificial pancreas system. Other artificial pancreas systems have been approved since 2016. NIDDK continues to support research into artificial pancreas systems and other technologies that may improve diabetes management.
Blood glucose management studies
NIDDK funded the landmark Diabetes Control and Complications Trial (DCCT). The study showed that participants with type 1 diabetes who kept their blood glucose levels close to normal greatly lowered their chances of developing eye, kidney, and nerve disease. A follow-up study, the ongoing Epidemiology of Diabetes Interventions and Complications (EDIC) study, has continued to follow DCCT participants since 1994. EDIC has shown that there are long-term benefits of early and intensive blood glucose management on slowing or preventing the development of health problems such as heart, eye, kidney, and nerve diseases. Findings from the DCCT and EDIC studies changed the way diabetes is treated worldwide, and they show that blood glucose control can help people with diabetes lead longer and healthier lives.
NIDDK also funded the Diabetes & Aging Study to research the effects of early blood glucose management and the development of diabetes health problems in people with type 2 diabetes. The study found that people with less effective diabetes management during the first year after being diagnosed with diabetes had a higher risk of diabetes complications and death.
The Treatment Options for Type 2 Diabetes in Adolescents and Youth (TODAY) study and a follow-up study, TODAY2, found that type 2 diabetes can be more difficult to treat and manage when it occurs in younger people. The TODAY studies, both funded by NIDDK, show the importance of early, intensive treatment and blood glucose management for children or adolescents diagnosed with type 2 diabetes.
References
Insulin, Medicines, & Other Diabetes Treatments
On this page:
- What medicines might I take for diabetes?
- What type of diabetes do I have?
- What are the different types of insulin?
- What are the different ways to take insulin?
- What oral medicines treat type 2 diabetes?
- What other injectable medicines treat diabetes?
- What should I know about side effects of diabetes medicines?
- What questions should I ask about my diabetes medicines?
- Do I have other treatment options for my diabetes?
- Clinical Trials for Insulin, Medicines, & Other Diabetes Treatments
Taking insulin or other diabetes medicines is often part of treating diabetes. In addition to making healthy food and beverage choices, getting physical activity, getting enough sleep, and managing stress, medicines can help you manage the disease. Some other treatment options are also available.
What medicines might I take for diabetes?
The medicine you take depends on the type of diabetes you have and how well the medicine controls your blood glucose levels, also called blood sugar levels. Other factors, such as any other health conditions you may have, medication costs, your insurance coverage and copays, access to care, and your lifestyle, may affect what diabetes medicine you take.
What type of diabetes do I have?
Type 1 diabetes
If you have type 1 diabetes, you must take insulin because your pancreas does not make it. You will need to take insulin several times during the day, including when you eat and drink, to control your blood glucose level.
There are different ways to take insulin. You can use a needle and syringe, an insulin pen, or an insulin pump. An artificial pancreas—also called an automated insulin delivery system—may be another option for some people.
Type 2 diabetes
Some people with type 2 diabetes can control their blood glucose level by making lifestyle changes. These lifestyle changes include consuming healthy meals and beverages, limiting calories if they have overweight or obesity, and getting physical activity.
Many people with type 2 diabetes need to take diabetes medicines as well. These medicines may include diabetes pills or medicines you inject, such as insulin. Over time, you may need more than one diabetes medicine to control your blood glucose level. Even if you do not take insulin, you may need it at special times, such as if you are pregnant or if you are in the hospital for treatment.
Gestational diabetes
If you have gestational diabetes, you can manage your blood glucose level by following a healthy eating plan and doing a moderate-intensity physical activity, such as brisk walking for 150 minutes, each week. If consuming healthy food and beverages and getting regular physical activity aren’t enough to keep your blood glucose level in your target range, a doctor will work with you and may recommend you take insulin. Insulin is safe to take while you are pregnant.
No matter what type of diabetes you have, taking diabetes medicines every day can feel like a burden sometimes. New medications and improved delivery systems can help make it easier to manage your blood glucose levels. Talk with your doctor to find out which medications and delivery systems will work best for you and fit into your lifestyle.
What are the different types of insulin?
Several types of insulin are available. Each type starts to work at a different speed, known as “onset,” and its effects last a different length of time, known as “duration.” Most types of insulin reach a peak, which is when they have the strongest effect. After the peak, the effects of the insulin wear off over the next few hours or so. Table 1 lists the different types of insulin, how fast they start to work, when they peak, and how long they last.
Table 1. Types of insulin and how they work1,2
| Insulin Type | How Fast It Starts to Work (onset) | When It Peaks | How Long It Lasts (duration) |
| rapid-acting/ ultra rapid-acting |
15 minutes | 1 hour | 2 to 4 hours (rapid) 5 to 7 hours (ultra) |
| rapid-acting, inhaled | 10 to 15 minutes | 30 minutes | 3 hours |
| regular, also called short-acting | 30 minutes | 2 to 3 hours | 3 to 6 hours |
| intermediate-acting | 2 to 4 hours | 4 to 12 hours | 12 to 18 hours |
| long-acting | 2 hours | does not peak | 24 hours |
| ultra long-acting | 6 hours | does not peak | 36 hours or longer |
Another type of insulin, called premixed insulin, is a combination of insulins listed in Table 1. Premixed insulin starts to work in 15 to 60 minutes and can last from 10 to 16 hours. The peak time varies depending on which insulins are mixed.
Your doctor will work with you to review your medication options. Talk with your doctor about your activity level, what you eat and drink, how well you manage your blood glucose levels, your age and lifestyle, and how long your body takes to absorb insulin.
Follow your doctor’s advice on when and how to take your insulin. If you're worried about the cost, talk with your doctor. Some types of insulin cost more than others. You can also find resources to get financial help for diabetes care.
What are the different ways to take insulin?
The way you take insulin may depend on your lifestyle, insurance plan, and preferences. Talk with your doctor about the options and which one is best for you. Most people with diabetes take insulin using a needle and syringe, insulin pen, or insulin pump. Inhalers and insulin jet injectors are less common ways to take insulin. Artificial pancreas systems are now approved by the U.S. Food and Drug Administration (FDA). Talk with your doctor to see if an artificial pancreas is an option for you.
Needle and syringe
You can give yourself insulin shots using a needle and syringe. You draw up your dose of insulin from the vial—or bottle—through the needle into the syringe. Insulin works fastest when you inject it in your belly, but your doctor may recommend alternating the spot where you inject it. Injecting insulin in the same spot repeatedly could cause the tissue to harden, making it harder to take shots in that area over time. Other spots you can inject insulin include your thigh, buttocks, or upper arm, but it may take longer for the insulin to work from those areas. Some people with diabetes who take insulin need 2 to 4 shots a day to reach their blood glucose targets. Others can take a single shot. Injection aids can help you give yourself the shots.

Pen
An insulin pen looks like a writing pen but has a needle for its point. Some insulin pens come filled with insulin and are disposable. Others have room for an insulin cartridge that you insert and replace after use. Many people find insulin pens easier to use, but they cost more than needles and syringes. You may want to consider using an insulin pen if you find it hard to fill the syringe while holding the vial or cannot read the markings on the syringe. Different pen types have features that can help with your injections. Some reusable pens have a memory function, which can recall dose amounts and timing. Other types of “connected” insulin pens can be programmed to calculate insulin doses and provide downloadable data reports, which can help you and your doctor adjust your insulin doses.

Pump
An insulin pump is a small machine that gives you steady doses of insulin throughout the day. You wear one type of pump outside your body on a belt or in a pocket or pouch. The insulin pump connects to a small plastic tube and a very small needle. You insert the plastic tube with a needle under your skin, then take out the needle. The plastic tube will stay inserted for several days while attached to the insulin pump. The machine pumps insulin through the tube into your body 24 hours a day and can be programmed to give you more or less insulin based on your needs. You can also give yourself doses of insulin through the pump at mealtimes.
Another type of pump has no tubes. This pump attaches directly to your skin with a self-adhesive pad and is controlled by a hand-held device. The plastic tube and pump device are changed every several days.

Inhaler
Another way to take insulin is by breathing powdered insulin into your mouth from an inhaler device. The insulin goes into your lungs and moves quickly into your blood. You may want to use an insulin inhaler to avoid using needles. Inhaled insulin is only for adults with type 1 or type 2 diabetes. Taking insulin with an inhaler is less common than using a needle and syringe.
Jet injector
A jet injector is a device that sends a fine spray of insulin into the skin at high pressure instead of using a needle to deliver the insulin. It is used less commonly than a needle and syringe or a pen.
Artificial pancreas
An artificial pancreas is a system of three devices that work together to mimic how a healthy pancreas controls blood glucose in the body. A continuous glucose monitor (CGM) tracks blood glucose levels every few minutes using a small sensor inserted under the skin that is held in place with an adhesive pad. The CGM wirelessly sends the information to a program on a smartphone or an insulin infusion pump. The program calculates how much insulin you need. The insulin infusion pump will adjust how much insulin is given from minute to minute to help keep your blood glucose level in your target range. An artificial pancreas is mainly used to help people with type 1 diabetes.
What oral medicines treat type 2 diabetes?
You may need to take medicines to manage your type 2 diabetes, in addition to consuming healthy foods and beverages and being physically active. You can take many diabetes medicines by mouth. These medicines are called oral medicines.
Most people with type 2 diabetes start with metformin pills. Metformin also comes as a liquid. Metformin helps your liver make less glucose and helps your body use insulin better. This drug may help you lose a small amount of weight.
Other oral medicines act in different ways to lower blood glucose levels. Combining two or three kinds of diabetes medicines can lower blood glucose levels better than taking just one medicine.
Read about different kinds of diabetes medicines (PDF, 2.8 MB) from the FDA.
What other injectable medicines treat diabetes?
Type 1 diabetes
If you have type 1 diabetes, your doctor may recommend you take other medicines, in addition to insulin, to help control your blood glucose. Some of these medicines work to slow how fast food and beverages move through your stomach. These medicines also slow down how quickly and how high your blood glucose levels rise after eating. Other medicines work to block certain hormones in your digestive system that raise blood glucose levels after meals or help the kidneys to remove more glucose from your blood.
Type 2 diabetes
Besides insulin, other types of injected medicines (PDF, 2.8 MB) are available that will keep your blood glucose level from rising too high after you eat or drink. These medicines, known as glucagon-like peptide-1 (GLP-1) receptor agonists,3 may make you feel less hungry and help you lose some weight. GLP-1 medicines are not substitutes for insulin.
What should I know about side effects of diabetes medicines?
Side effects are problems that result from taking a medicine. Some diabetes medicines can cause hypoglycemia, also called low blood glucose, if you don’t balance your medicines with food and activity.
Ask your doctor whether your diabetes medicine can cause hypoglycemia or other side effects, such as upset stomach and weight gain. Aim to take your diabetes medicines as your doctor instructs you, to help prevent side effects and diabetes problems.
Do I have other treatment options for my diabetes?
If medicines and lifestyle changes are not enough to manage your diabetes, there are other treatments that might help you. These treatments include weight-loss (bariatric) surgery for certain people with type 1 or type 2 diabetes, or pancreatic islet transplantation for some people with type 1 diabetes.
Weight-loss surgery
Weight-loss surgery are operations that help you lose weight by making changes to your digestive system. Weight-loss surgery is also called bariatric or metabolic surgery.
This type of surgery may help some people who have obesity and type 2 diabetes lose a large amount of weight and bring their blood glucose levels back to a healthy range. How long the improved response lasts can vary by patient, type of weight-loss surgery, and the amount of weight the person lost. Other factors include how long a person had diabetes and whether the person used insulin. Some people with type 2 diabetes may no longer need to use diabetes medicines after weight-loss surgery.4
Researchers are studying whether weight-loss surgery can help control blood glucose levels in people with type 1 diabetes who have obesity.5
Pancreatic islet transplantation
Pancreatic islet transplantation is a treatment for type 1 diabetes in people who struggle to manage their blood glucose levels. Pancreatic islets are clusters of cells in the pancreas that make the hormone insulin. In type 1 diabetes, the body’s immune system attacks these cells. A pancreatic islet transplantation replaces destroyed islets with new islets from a deceased donor. The new islets make and release insulin.
Clinical Trials for Insulin, Medicines, & Other Diabetes Treatments
The NIDDK conducts and supports clinical trials in many diseases and conditions, including diabetes. The trials look to find new ways to prevent, detect, or treat disease and improve quality of life.
What are clinical trials for insulin, medicines, and other diabetes treatments?
Clinical trials—and other types of clinical studies—are part of medical research and involve people like you. When you volunteer to take part in a clinical study, you help health care professionals and researchers learn more about disease and improve health care for people in the future.
Find out if clinical trials are right for you.
Researchers are studying many aspects of diabetes medicines, including
- new types of insulin
- the most effective times to take diabetes medicines
- new types of monitoring devices and delivery systems
Watch a video of NIDDK Director Dr. Griffin P. Rodgers explaining the importance of participating in clinical trials.
What clinical trials for insulin, medicines, and other diabetes treatments are looking for participants?
You can view a filtered list of clinical studies on insulin, medicines, and other diabetes treatments covered in this health topic that are federally funded, open, and recruiting at
ClinicalTrials.gov. You can expand or narrow the list to include clinical studies from industry, universities, and individuals; however, the National Institutes of Health does not review these studies and cannot ensure they are safe. Always talk with your health care provider before you participate in a clinical study.
References
Healthy Living with Diabetes
On this page:
- How can I plan what to eat or drink when I have diabetes?
- How can physical activity help manage my diabetes?
- What can I do to reach or maintain a healthy weight?
- Should I quit smoking?
- How can I take care of my mental health?
- Clinical Trials for Healthy Living with Diabetes
Healthy living is a way to manage diabetes. To have a healthy lifestyle, take steps now to plan healthy meals and snacks, do physical activities, get enough sleep, and quit smoking or using tobacco products.
Healthy living may help keep your body’s blood pressure, cholesterol, and blood glucose level, also called blood sugar level, in the range your primary health care professional recommends. Your primary health care professional may be a doctor, a physician assistant, or a nurse practitioner. Healthy living may also help prevent or delay health problems from diabetes that can affect your heart, kidneys, eyes, brain, and other parts of your body.
Making lifestyle changes can be hard, but starting with small changes and building from there may benefit your health. You may want to get help from family, loved ones, friends, and other trusted people in your community. You can also get information from your health care professionals.
How can I plan what to eat or drink when I have diabetes?
What you choose to eat, how much you eat, and when you eat are parts of a meal plan. Having healthy foods and drinks can help keep your blood glucose, blood pressure, and cholesterol levels in the ranges your health care professional recommends. If you have overweight or obesity, a healthy meal plan—along with regular physical activity, getting enough sleep, and other healthy behaviors—may help you reach and maintain a healthy weight. In some cases, health care professionals may also recommend diabetes medicines that may help you lose weight, or weight-loss surgery, also called metabolic and bariatric surgery.
Choose healthy foods and drinks
There is no right or wrong way to choose healthy foods and drinks that may help manage your diabetes. Healthy meal plans for people who have diabetes may include
Try to choose foods that include nutrients such as vitamins, calcium, fiber, and healthy fats. Also try to choose drinks with little or no added sugar, such as tap or bottled water, low-fat or non-fat milk, and unsweetened tea, coffee, or sparkling water.
Try to plan meals and snacks that have fewer
- foods high in saturated fat
- foods high in sodium, a mineral found in salt
- sugary foods, such as cookies and cakes, and sweet drinks, such as soda, juice, flavored coffee, and sports drinks
Your body turns carbohydrates, or carbs, from food into glucose, which can raise your blood glucose level. Some fruits, beans, and starchy vegetables—such as potatoes and corn—have more carbs than other foods. Keep carbs in mind when planning your meals.
You should also limit how much alcohol you drink. If you take insulin or certain diabetes medicines, drinking alcohol can make your blood glucose level drop too low, which is called hypoglycemia. If you do drink alcohol, be sure to eat food when you drink and remember to check your blood glucose level after drinking. Talk with your health care team about your alcohol-drinking habits.
 Try to choose foods that include nutrients such as vitamins, calcium, fiber, and healthy fats.
Try to choose foods that include nutrients such as vitamins, calcium, fiber, and healthy fats.
Find the best times to eat or drink
Talk with your health care professional or health care team about when you should eat or drink. The best time to have meals and snacks may depend on
- what medicines you take for diabetes
- what your level of physical activity or your work schedule is
- whether you have other health conditions or diseases
Ask your health care team if you should eat before, during, or after physical activity. Some diabetes medicines, such as sulfonylureas or insulin, may make your blood glucose level drop too low during exercise or if you skip or delay a meal.
Plan how much to eat or drink
You may worry that having diabetes means giving up foods and drinks you enjoy. The good news is you can still have your favorite foods and drinks, but you might need to have them in smaller portions or enjoy them less often.
For people who have diabetes, carb counting and the plate method are two common ways to plan how much to eat or drink. Talk with your health care professional or health care team to find a method that works for you.
Carb counting
Carbohydrate counting, or carb counting, means planning and keeping track of the amount of carbs you eat and drink in each meal or snack. Not all people with diabetes need to count carbs. However, if you take insulin, counting carbs can help you know how much insulin to take.
Plate method
The plate method helps you control portion sizes without counting and measuring. This method divides a 9-inch plate into the following three sections to help you choose the types and amounts of foods to eat for each meal.
- Nonstarchy vegetables—such as leafy greens, peppers, carrots, or green beans—should make up half of your plate.
- Carb foods that are high in fiber—such as brown rice, whole grains, beans, or fruits—should make up one-quarter of your plate.
- Protein foods—such as lean meats, fish, dairy, or tofu or other soy products—should make up one quarter of your plate.
If you are not taking insulin, you may not need to count carbs when using the plate method.
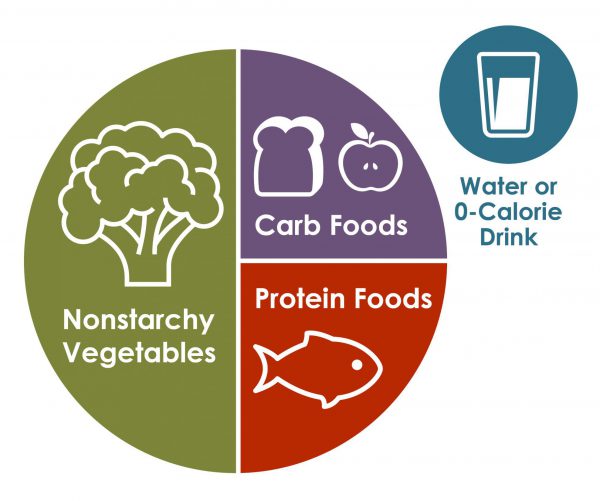 Source: Centers for Disease Control and Prevention The plate method may help you control your blood glucose without counting carbs.
Source: Centers for Disease Control and Prevention The plate method may help you control your blood glucose without counting carbs.
Work with your health care team to create a meal plan that works for you. You may want to have a diabetes educator or a registered dietitian on your team. A registered dietitian can provide medical nutrition therapy, which includes counseling to help you create and follow a meal plan. Your health care team may be able to recommend other resources, such as a healthy lifestyle coach, to help you with making changes. Ask your health care team or your insurance company if your benefits include medical nutrition therapy or other diabetes care resources.
Talk with your health care professional before taking dietary supplements
There is no clear proof that specific foods, herbs, spices, or dietary supplements—such as vitamins or minerals—can help manage diabetes. Your health care professional may ask you to take vitamins or minerals if you can’t get enough from foods. Talk with your health care professional before you take any supplements, because some may cause side effects or affect how well your diabetes medicines work.
How can physical activity help manage my diabetes?
Research shows that regular physical activity helps people manage their diabetes and stay healthy. Benefits of physical activity may include
- lower blood glucose, blood pressure, and cholesterol levels
- better heart health
- healthier weight
- better mood and sleep
- better balance and memory
Talk with your health care professional before starting a new physical activity or changing how much physical activity you do. They may suggest types of activities based on your ability, schedule, meal plan, interests, and diabetes medicines. Your health care professional may also tell you the best times of day to be active or what to do if your blood glucose level goes out of the range recommended for you.
 Physical activity may help you manage your diabetes and stay healthy.
Physical activity may help you manage your diabetes and stay healthy.
Do different types of physical activity
People with diabetes can be active, even if they take insulin or use technology such as insulin pumps.
Try to do different kinds of activities. While being more active may have more health benefits, any physical activity is better than none. Start slowly with activities you enjoy. You may be able to change your level of effort and try other activities over time. Having a friend or family member join you may help you stick to your routine.
The physical activities you do may need to be different if you are age 65 or older, are pregnant, or have a disability or health condition. Physical activities may also need to be different for children and teens. Ask your health care professional or health care team about activities that are safe for you.
Aerobic activities
Aerobic activities make you breathe harder and make your heart beat faster. You can try walking, dancing, wheelchair rolling, or swimming. Most adults should try to get at least 150 minutes of moderate-intensity physical activity each week. Aim to do 30 minutes a day on most days of the week. You don’t have to do all 30 minutes at one time. You can break up physical activity into small amounts during your day and still get the benefit.1
Strength training or resistance training
Strength training or resistance training may make your muscles and bones stronger. You can try lifting weights or doing other exercises such as wall pushups or arm raises. Try to do this kind of training two times a week.1
Balance and stretching activities
Balance and stretching activities may help you move better and have stronger muscles and bones. You may want to try standing on one leg or stretching your legs when sitting on the floor. Try to do these kinds of activities two or three times a week.1
Some activities that need balance may be unsafe for people with nerve damage or vision problems caused by diabetes. Ask your health care professional or health care team about activities that are safe for you.
 If you can, try to do different types of physical activities. Start slowly with activities you enjoy.
If you can, try to do different types of physical activities. Start slowly with activities you enjoy.
Stay safe during physical activity
Staying safe during physical activity is important. Here are some tips to keep in mind.
Drink liquids
Drinking liquids helps prevent dehydration, or the loss of too much water in your body. Drinking water is a way to stay hydrated. Sports drinks often have a lot of sugar and calories, and you don’t need them for most moderate physical activities.
Avoid low blood glucose
Check your blood glucose level before, during, and right after physical activity. Physical activity often lowers the level of glucose in your blood. Low blood glucose levels may last for hours or days after physical activity. You are most likely to have low blood glucose if you take insulin or some other diabetes medicines, such as sulfonylureas.
Ask your health care professional if you should take less insulin or eat carbs before, during, or after physical activity. Low blood glucose can be a serious medical emergency that must be treated right away. Take steps to protect yourself. You can learn how to treat low blood glucose, let other people know what to do if you need help, and use a medical alert bracelet.
Avoid high blood glucose and ketoacidosis
Taking less insulin before physical activity may help prevent low blood glucose, but it may also make you more likely to have high blood glucose. If your body does not have enough insulin, it can’t use glucose as a source of energy and will use fat instead. When your body uses fat for energy, your body makes chemicals called ketones.
High levels of ketones in your blood can lead to a condition called diabetic ketoacidosis (DKA). DKA is a medical emergency that should be treated right away. DKA is most common in people with type 1 diabetes. Occasionally, DKA may affect people with type 2 diabetes who have lost their ability to produce insulin. Ask your health care professional how much insulin you should take before physical activity, whether you need to test your urine for ketones, and what level of ketones is dangerous for you.
Take care of your feet
People with diabetes may have problems with their feet because high blood glucose levels can damage blood vessels and nerves. To help prevent foot problems, wear comfortable and supportive shoes and take care of your feet before, during, and after physical activity.
 Take care of your feet before, during, and after physical activity.
Take care of your feet before, during, and after physical activity.
What can I do to reach or maintain a healthy weight?
If you have diabetes, managing your weight may bring you several health benefits. Ask your health care professional or health care team if you are at a healthy weight or if you should try to lose weight.
If you are an adult with overweight or obesity, work with your health care team to create a weight-loss plan. Losing 5% to 7% of your current weight may help you prevent or improve some health problems and manage your blood glucose, cholesterol, and blood pressure levels.2 If you are worried about your child’s weight and they have diabetes, talk with their health care professional before your child starts a new weight-loss plan.
You may be able to reach and maintain a healthy weight by
- following a healthy meal plan
- consuming fewer calories
- being physically active
- getting 7 to 8 hours of sleep each night3
If you have type 2 diabetes, your health care professional may recommend diabetes medicines that may help you lose weight.
Online tools such as the Body Weight Planner may help you create eating and physical activity plans. You may want to talk with your health care professional about other options for managing your weight, including joining a weight-loss program that can provide helpful information, support, and behavioral or lifestyle counseling. These options may have a cost, so make sure to check the details of the programs.
Your health care professional may recommend weight-loss surgery if you aren’t able to reach a healthy weight with meal planning, physical activity, and taking diabetes medicines that help with weight loss.
If you are pregnant, trying to lose weight may not be healthy. However, you should ask your health care professional whether it makes sense to monitor or limit your weight gain during pregnancy.
Should I quit smoking?
Both diabetes and smoking—including using tobacco products and e-cigarettes—cause your blood vessels to narrow. Both diabetes and smoking increase your risk of having a heart attack or stroke, nerve damage, kidney disease, eye disease, or amputation. Secondhand smoke can also affect the health of your family or others who live with you.
If you smoke or use other tobacco products, stop. Ask for help. You don’t have to do it alone.
How can I take care of my mental health?
Feeling stressed, sad, or angry can be common for people with diabetes. Managing diabetes or learning to cope with new information about your health can be hard. People with chronic illnesses such as diabetes may develop anxiety or other mental health conditions.
Learn healthy ways to lower your stress, and ask for help from your health care team or a mental health professional. While it may be uncomfortable to talk about your feelings, finding a health care professional whom you trust and want to talk with may help you
- lower your feelings of stress, depression, or anxiety
- manage problems sleeping or remembering things
- see how diabetes affects your family, school, work, or financial situation
Ask your health care team for mental health resources for people with diabetes.
Sleeping too much or too little may raise your blood glucose levels. Your sleep habits may also affect your mental health and vice versa. People with diabetes and overweight or obesity can also have other health conditions that affect sleep, such as sleep apnea, which can raise your blood pressure and risk of heart disease.
 Having diabetes can be stressful. Talk with your health care professional or health care team if you need help.
Having diabetes can be stressful. Talk with your health care professional or health care team if you need help.
Clinical Trials for Healthy Living with Diabetes
NIDDK conducts and supports clinical trials in many diseases and conditions, including diabetes. The trials look to find new ways to prevent, detect, or treat disease and improve quality of life.
What are clinical trials for healthy living with diabetes?
Clinical trials—and other types of clinical studies—are part of medical research and involve people like you. When you volunteer to take part in a clinical study, you help health care professionals and researchers learn more about disease and improve health care for people in the future.
Researchers are studying many aspects of healthy living for people with diabetes, such as
- how changing when you eat may affect body weight and metabolism
- how less access to healthy foods may affect diabetes management, other health problems, and risk of dying
- whether low-carbohydrate meal plans can help lower blood glucose levels
- which diabetes medicines are more likely to help people lose weight
Find out if clinical trials are right for you.
Watch a video of NIDDK Director Dr. Griffin P. Rodgers explaining the importance of participating in clinical trials.
What clinical trials for healthy living with diabetes are looking for participants?
You can view a filtered list of clinical studies on healthy living with diabetes that are federally funded, open, and recruiting at ClinicalTrials.gov. You can expand or narrow the list to include clinical studies from industry, universities, and individuals; however, the National Institutes of Health does not review these studies and cannot ensure they are safe for you. Always talk with your primary health care professional before you participate in a clinical study.
References
Preventing Diabetes Problems
Diabetes can lead to serious health problems such as heart disease, vision problems, nerve damage, and kidney disease. Learn more about preventing these diabetes problems and managing your diabetes.
Heart Disease & Stroke
Diabetes can damage blood vessels and lead to heart disease and stroke. You can do a lot to prevent heart disease and stroke by managing your blood glucose, blood pressure, and cholesterol levels; and by not smoking.
Low Blood Glucose (Hypoglycemia)
Hypoglycemia occurs when your blood glucose drops too low. Certain diabetes medicines make low blood glucose more likely. You can prevent hypoglycemia by following your meal plan and balancing your physical activity, food, and medicines. Testing your blood glucose regularly can also help prevent hypoglycemia.
Diabetic Neuropathy
Diabetic neuropathy is nerve damage that can result from diabetes. Different types of nerve damage affect different parts of your body. Managing your diabetes can help prevent nerve damage that affects your feet and limbs, and organs such as your heart.
Foot Problems
Diabetes can cause nerve damage and poor blood flow, which can lead to serious foot problems. Common foot problems, such as a callus, can lead to pain or an infection that makes it hard to walk. Get a foot checkup at each visit with your health care team.
Kidney Disease
Diabetic kidney disease, also called diabetic nephropathy, is kidney disease caused by diabetes. You can help protect your kidneys by managing your diabetes and meeting your blood pressure goals.
Eye Disease
Diabetes can damage your eyes and lead to low vision and blindness. The best way to prevent eye disease is to manage your blood glucose, blood pressure, and cholesterol; and to not smoke. Also, have a dilated eye exam at least once a year.
Gum Disease & Other Dental Problems
Diabetes can lead to problems in your mouth, such as infection, gum disease, or dry mouth. To help keep your mouth healthy, manage your blood glucose, brush your teeth twice a day, see your dentist at least once a year, and don’t smoke.
Sexual & Bladder Problems
Sexual and bladder problems are more common in people with diabetes. Problems like erectile dysfunction, loss of interest in sex, bladder leaks, and retained urine can happen if diabetes damages your blood vessels and nerves. Treatments are available to help control symptoms and restore intimacy.
Cancer & Diabetes
Diabetes is linked to some types of cancer. Many risk factors for cancer and for diabetes are the same. Not smoking and getting recommended cancer screenings can help prevent cancer.
Dementia & Diabetes
High blood glucose increases the chance of developing dementia. Tell your doctor if you are forgetful because dementia can make it hard to manage your diabetes.
Depression & Diabetes
Depression is common among people with a chronic, or long-term, illness such as diabetes. Depression can be treated so tell your doctor if you feel sad, hopeless, or anxious.
Sleep Apnea & Diabetes
People who have sleep apnea—when you stop breathing for short periods during sleep—are more likely to develop type 2 diabetes. Sleep apnea also can make diabetes worse. Treatment for sleep apnea can help.
Clinical Trials
The National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) and other components of the National Institutes of Health (NIH) conduct and support research into many diseases and conditions. The NIDDK is the primary institute at the NIH that funds diabetes research, including clinical trials.
What are clinical trials for diabetes?
Clinical trials are part of clinical research and at the heart of all medical advances. Clinical trials look at new ways to prevent, detect, or treat disease. Scientists are conducting research to learn more about diabetes, including the following studies
- The Glycemia Reduction Approaches in Diabetes: A Comparative Effectiveness Study (GRADE) is following more than 5,000 people across the country who have type 2 diabetes to find out which combination of two diabetes medicines is best for blood glucose, also called blood sugar, management; has the fewest side effects; and is the most helpful for overall health in long-term diabetes treatment.
- TrialNet is conducting research studies around the world, including risk screening for relatives of people with type 1 diabetes, monitoring for people at risk, and innovative clinical trials aimed at slowing down or stopping the disease.
Researchers also use clinical trials to look at other aspects of care, such as improving the quality of life for people with chronic illnesses. Find out if clinical trials are right for you.
Watch a video of NIDDK Director Dr. Griffin P. Rodgers explaining the importance of participating in clinical trials.
What clinical trials for diabetes are open?
Below is a list of selected clinical trials that are currently open and recruiting, but you can expand or narrow your search.
- Type 1 diabetes—includes studies funded by the NIH or other U.S. Government agencies
- Type 2 diabetes—includes studies funded by the NIH or other U.S. Government agencies
- Gestational diabetes—includes studies funded by the NIH; other U.S. Government agencies; and individuals, universities, or other organizations
You can also search ClinicalTrials.gov to find studies on other types of diabetes or on specific conditions linked to diabetes.
What have we learned about diabetes from NIDDK-funded research?
The NIDDK has supported many research projects to learn more about diabetes. For example
- Look AHEAD: Action for Health in Diabetes. The Look AHEAD study showed that people who were overweight or had obesity and had type 2 diabetes can lose weight and maintain that weight loss through a program of healthy eating and increased physical activity. The study also showed that weight loss provides added health benefits, such as better physical mobility and improved blood glucose, blood pressure, and cholesterol levels. The trial has been extended to study the long-term results of weight loss through healthy eating and physical activity programs in older adults with type 2 diabetes.
- Diabetes Control and Complications Trial (DCCT) and Epidemiology of Diabetes Interventions and Complications (EDIC). The DCCT showed that intensive treatment with insulin to maintain blood glucose levels as close to normal as safely possible greatly lowered participants’ chances of developing eye, nerve, and kidney disease. The EDIC study has continued to follow DCCT participants for the past 20+ years. EDIC has shown that there are long-term benefits of early and intensive blood glucose control for the future development of diabetes-related complications such as heart, kidney, nerve, and eye disease; and that early and intensive control also lengthens life.
- Diabetes Prevention Program (DPP) and Diabetes Prevention Program Outcomes Study (DPPOS). The DPP showed that people who are at high risk for type 2 diabetes can prevent or delay the disease by making lifestyle changes that include weight loss through dietary changes and increased physical activity. Taking metformin, a safe and effective generic medicine used to treat diabetes, was also found to prevent the disease, although to a lesser degree. The DPPOS has continued to follow DPP participants to see if the lifestyle changes they made during the DPP or taking metformin continues to prevent or delay type 2 diabetes over time. To date, the DPPOS has shown that people can prevent or delay type 2 diabetes for at least 15 years with lifestyle changes or metformin.
This content is provided as a service of the National Institute of Diabetes and Digestive and Kidney Diseases
(NIDDK), part of the National Institutes of Health. NIDDK translates and disseminates research findings to increase knowledge and understanding about health and disease among patients, health professionals, and the public. Content produced by NIDDK is carefully reviewed by NIDDK scientists and other experts.
